Urinary tract infections (UTIs) are a surprisingly common nuisance for many women, often causing discomforting symptoms like burning sensations during urination, frequent urges to go, and even abdominal pain. While frequently associated with sexual activity or poor hygiene, the causes behind these infections can be more complex than typically understood. Increasingly, women are questioning whether hormonal fluctuations – and specifically, hormonal birth control methods – play a role in their susceptibility to UTIs. This is understandable given the significant impact hormones have on various bodily systems, including the urinary tract and immune responses. Understanding this potential link requires delving into how different types of hormonal pills affect the body and what research suggests about their connection to UTI development.
The relationship between hormonal birth control and UTIs isn’t straightforward. It’s not a case of pills causing infections directly in most instances, but rather influencing factors that can make women more vulnerable. These factors include changes to vaginal flora (the naturally occurring bacteria), alterations in the immune system, and even shifts in bladder function. The key is recognizing that hormonal fluctuations – natural or induced by medication – are a normal part of a woman’s reproductive life and often impact overall health in multifaceted ways. This article will explore these connections, offering insights into what current research reveals and empowering women to make informed decisions about their healthcare.
Hormonal Birth Control & Vaginal Microbiome Disruption
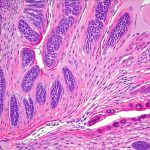
The vaginal microbiome is a delicate ecosystem composed of various bacteria, most notably Lactobacilli. These “good” bacteria maintain an acidic pH level which inhibits the growth of harmful pathogens that can lead to infections like UTIs and bacterial vaginosis (BV). Hormonal fluctuations, especially those induced by birth control pills containing estrogen, can significantly alter this balance. – Estrogen increases glycogen stores in the vaginal walls. While seemingly beneficial, this provides more “food” for bacteria – both good and bad. – Higher estrogen levels can also reduce the dominance of Lactobacilli, creating an environment where opportunistic pathogens like E. coli (a common UTI culprit) can thrive. This isn’t to say all hormonal birth control causes microbiome disruption; it varies based on formulation and individual response. Progestin-only pills, for example, generally have less impact on vaginal flora compared to combined estrogen-progestin pills.
The link between a disrupted microbiome and UTIs is well-established. A healthy vaginal ecosystem acts as the first line of defense against ascending infections – meaning preventing bacteria from traveling up the urethra into the bladder. When Lactobacilli are reduced, this protective barrier weakens, increasing the risk of UTI development. It’s important to note that BV itself doesn’t always cause a UTI, but it significantly increases the likelihood because it creates an environment conducive for UTI-causing bacteria to flourish and spread. Some research suggests that women who experience frequent UTIs may benefit from strategies aimed at restoring and maintaining a healthy vaginal microbiome, such as probiotics specifically formulated for vaginal health (though more robust evidence is still needed). Understanding how environmental toxins can also impact urinary health provides further context to overall wellness.
This disruption isn’t limited to combined pills; even hormonal IUDs releasing progestin can indirectly impact the vaginal microbiome over time. While these effects are often mild, they contribute to the overall complexity of understanding UTI susceptibility in women using hormonal contraception. The individual response to these changes also plays a critical role – factors like diet, stress levels, and existing health conditions can all influence how a woman’s body reacts to hormonal fluctuations.
Estrogen’s Impact on Immune Function
Beyond the vaginal microbiome, estrogen has a profound impact on the immune system, influencing both local and systemic immunity. – Estrogen generally enhances certain aspects of the immune response, making it more efficient at fighting off infections. However, this isn’t always straightforward. High levels of estrogen can also suppress some immune functions, potentially weakening the body’s ability to clear an existing infection or prevent a new one from taking hold. This is particularly relevant in the context of UTIs because the urinary tract relies on a robust immune response to combat invading bacteria. – Estrogen affects the production and function of key immune cells like neutrophils and macrophages – both crucial for fighting off bacterial infections. These cells are responsible for engulfing and destroying pathogens, but their activity can be modulated by estrogen levels.
The relationship between estrogen and immunity is incredibly complex and isn’t fully understood. While some studies suggest that higher estrogen levels might improve the body’s initial response to infection, others indicate they could potentially hinder long-term immune memory or increase susceptibility to certain types of infections. The type of estrogen (natural versus synthetic), dosage, and individual variations all play a role in determining how these effects manifest. This is why some women may experience increased UTI frequency when starting or changing hormonal birth control methods, while others don’t notice any difference at all. Can hemoglobin be a sign of something more serious? Knowing the signs is crucial.
Furthermore, the immune system isn’t isolated; it interacts closely with other bodily systems. Hormonal changes can also affect stress levels and sleep patterns, both of which have a significant impact on immune function. Therefore, managing stress and prioritizing adequate rest are essential components of maintaining a healthy immune system – particularly for women using hormonal contraception.
Bladder Function & Hormonal Influence
The urinary bladder isn’t just a storage sac; it’s a dynamic organ with complex neurological control and muscle function. Estrogen receptors are present in the bladder, suggesting that estrogen can directly influence its operation. – Estrogen plays a role in maintaining the integrity of the bladder lining (the urothelium) and regulating the muscles responsible for bladder emptying. Fluctuations in estrogen levels can potentially lead to changes in bladder capacity, urinary frequency, and even urgency – symptoms often associated with UTIs, although not necessarily indicative of an actual infection. – Some studies suggest that lower estrogen levels (like those experienced during menopause or with certain hormonal birth control formulations) can weaken the bladder muscles, making it more difficult to completely empty the bladder. This residual urine can then become a breeding ground for bacteria, increasing the risk of UTI development.
However, the connection between estrogen and bladder function is still being investigated. It’s likely that other factors – such as pelvic floor muscle strength, hydration levels, and pre-existing medical conditions – also play significant roles in determining overall bladder health. Importantly, frequent urinary symptoms don’t automatically equal a UTI. Many women experience similar symptoms due to non-infectious causes like overactive bladder syndrome or interstitial cystitis. It’s crucial to consult with a healthcare professional for accurate diagnosis and appropriate treatment. Can electrolyte imbalance present in urine indicate underlying health issues?
The type of hormonal birth control also matters here. Pills with varying estrogen dosages can have different effects on bladder function, and some formulations may be more likely to cause urinary side effects than others. Women experiencing changes in their urinary habits after starting or switching hormonal contraception should discuss these concerns with their doctor. Can cystitis actually be caused by birth control? It’s a common question among women.
It’s important to reiterate that this information isn’t intended as medical advice. If you are concerned about UTIs or the potential impact of hormonal birth control, please consult with a healthcare provider for personalized guidance and evaluation. Can UTI pain be related to bowel movements? Understanding this connection can help manage symptoms. Additionally, urinalysis in veterinary medicine demonstrates the broad applications of urine testing for health assessment.