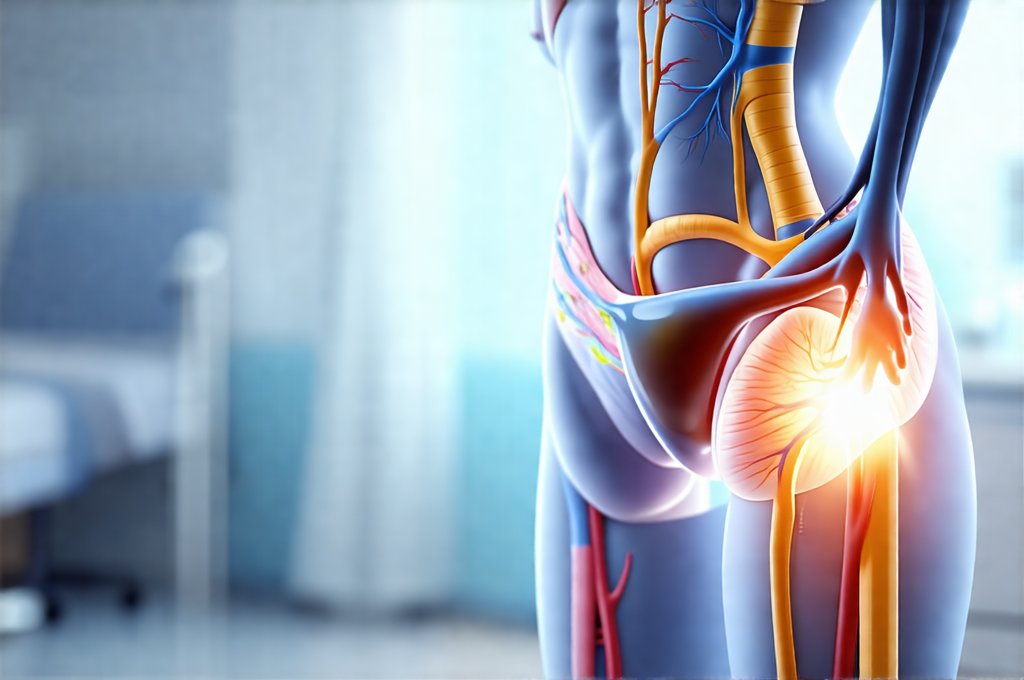
Urinary tract infections (UTIs) are incredibly common, affecting millions of people each year, particularly women. While antibiotics are often effective in clearing up the initial infection, the period after completing a course of antibiotics is crucial for restoring gut and vaginal health, preventing recurrence, and minimizing potential side effects. Many individuals understandably focus on eradicating the UTI itself, overlooking the importance of post-antibiotic care. This can lead to lingering discomfort, an increased susceptibility to future infections, or even broader health issues related to disrupted microbial balance.
The reason for this often stems from antibiotics’ non-selective nature – they don’t just target the bacteria causing the infection; they also impact beneficial microbes in the gut and vaginal microbiome. These ‘good’ bacteria play vital roles in digestion, immunity, and protection against opportunistic pathogens. Disrupting these ecosystems can have far-reaching consequences, making a proactive approach to post-UTI recovery essential. This article will explore what steps to take – and what to avoid – after finishing antibiotics for a UTI to support your body’s natural healing processes and reduce the risk of future problems.
Restoring Gut & Vaginal Health
Antibiotics are notorious for wiping out both harmful and beneficial bacteria. The gut microbiome, in particular, suffers significantly during antibiotic treatment. This disruption can lead to digestive issues like diarrhea, bloating, and abdominal pain. More seriously, it weakens the body’s natural defenses, making you more vulnerable to other infections – including recurrent UTIs. Similarly, the vaginal microbiome, dominated by Lactobacilli species, is crucial for maintaining a healthy pH balance that prevents harmful bacteria from flourishing. Antibiotics can diminish these protective bacteria, increasing the risk of bacterial vaginosis and yeast infections.
Therefore, prioritizing gut and vaginal health post-antibiotic treatment is paramount. This doesn’t necessarily mean rushing to take probiotics immediately; timing matters (more on that later). Instead, focus initially on a diet that supports microbial recovery. Avoiding processed foods, sugary drinks, and excessive alcohol are key. Incorporating fermented foods – like yogurt (with live cultures), kefir, sauerkraut, kimchi, and kombucha – can gradually reintroduce beneficial bacteria naturally. These foods provide probiotics and prebiotics (fibers that feed the good bacteria already present in your gut).
Rebuilding a healthy vaginal microbiome requires similar considerations. Avoid douching at all costs; it disrupts the natural balance of flora. Opt for breathable cotton underwear and avoid tight-fitting clothing. Consider discussing probiotic supplementation specifically formulated for vaginal health with your healthcare provider, but remember that probiotics aren’t a one-size-fits-all solution. The best approach is tailored to individual needs and circumstances. If you are concerned about recurring infections, it may be helpful to explore what to do if your UTI keeps coming back after sex.
Dietary Considerations Post-Antibiotics
Diet plays an incredibly significant role in the recovery process after antibiotic use. It’s not just about adding “good” foods; it’s also about avoiding things that can further exacerbate imbalances or hinder healing. A cornerstone of post-antibiotic dietary support is increasing fiber intake. Fiber acts as a prebiotic, nourishing the beneficial bacteria in your gut and aiding their regrowth. Excellent sources include fruits (especially berries), vegetables, whole grains, and legumes.
Furthermore, focusing on anti-inflammatory foods can help soothe the digestive system and reduce overall inflammation caused by the infection and antibiotic treatment. Foods rich in omega-3 fatty acids – like salmon, flaxseeds, and walnuts – are beneficial. Similarly, incorporating spices with anti-inflammatory properties, such as turmeric and ginger, can provide additional support. Hydration is also critical; drinking plenty of water helps flush out toxins and supports optimal gut function.
Conversely, several dietary factors should be minimized or avoided:
– Sugary foods and drinks: These feed harmful bacteria and suppress the immune system.
– Processed foods: Often lacking in essential nutrients and containing additives that can further disrupt gut health.
– Excessive caffeine & alcohol: These can irritate the digestive system and hinder recovery.
– Greasy or fried foods: Difficult to digest and can exacerbate inflammation. Understanding what to avoid during a UTI flare-up is also key for overall management.
Avoiding Harsh Soaps & Irritants
The skin around the urethra and vagina is particularly sensitive, and harsh soaps, detergents, and feminine hygiene products can disrupt the delicate balance of the microbiome. After antibiotic use, this sensitivity is amplified. Avoid using scented soaps, body washes, or wipes in the genital area. Opt for gentle, fragrance-free cleansers specifically designed for sensitive skin – or simply water.
This extends to laundry detergent as well. Switch to a hypoallergenic, fragrance-free detergent to wash your underwear and bedding. Residue from harsh detergents can irritate the skin and contribute to discomfort. Similarly, avoid using heavily scented lotions or perfumes in the genital area. The goal is to minimize any potential irritants that could further disrupt the microbiome or cause inflammation.
It’s also important to be mindful of certain personal care products like bubble baths and douches. These are notorious for stripping away natural oils and disrupting the vaginal pH balance, increasing the risk of infection. Stick to plain water for bathing and avoid douching entirely.
Timing Probiotic & Prebiotic Supplementation
The timing of probiotic and prebiotic supplementation is a surprisingly nuanced topic. While it’s tempting to start taking probiotics immediately after finishing antibiotics, this isn’t always the best approach. Antibiotics are designed to kill bacteria – including those in your probiotic supplements! Taking them simultaneously can render the probiotics ineffective. Instead, wait at least 2-3 hours after your last dose of antibiotic before starting a probiotic supplement.
When choosing a probiotic, look for one that contains multiple strains of Lactobacilli and Bifidobacteria, specifically those known to support urinary tract health. However, remember that probiotics are not a magic bullet. They work best when combined with a healthy diet and lifestyle. Prebiotics can be taken alongside probiotics to further enhance their effectiveness by providing food for the beneficial bacteria.
Consider cycling probiotic supplementation – taking them for a few weeks or months, then giving your gut a break. Long-term continuous use of probiotics may lead to dependence and reduced natural microbial diversity. Again, consulting with a healthcare professional is crucial to determine the appropriate probiotic strain and dosage for your individual needs. If you experience recurring symptoms, it’s important to understand how to avoid flare-ups after a UTI episode. Additionally, be aware of the risks associated with how to avoid antibiotic resistance in UTI treatment.
The information provided in this article is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.