The common cold, an almost universal experience, is typically associated with symptoms like a runny nose, sore throat, and fatigue. For many women, however, a seemingly innocuous cold can be accompanied by – or even trigger – a frustrating and often debilitating symptom: bladder pain. This connection isn’t always immediately obvious, leading to confusion and sometimes dismissal of the issue as simply “part of being sick.” Understanding why this happens requires delving into the intricate relationship between the immune system, inflammation, and the sensitive nature of the urinary tract, particularly in women. It’s a complex interplay, often involving more than just a direct physical link, and recognizing it is crucial for effective management and seeking appropriate care.
The vulnerability to experiencing bladder pain during or after a cold stems from several factors unique to female anatomy and physiology. Women are statistically more prone to urinary tract infections (UTIs), which can be exacerbated by immune system fluctuations accompanying a cold. Furthermore, the pelvic region contains a complex network of nerves, making it susceptible to referred pain – meaning discomfort originating elsewhere in the body can manifest as bladder pain. Hormonal changes also play a role, potentially increasing sensitivity during certain phases of the menstrual cycle or menopause and influencing how the body responds to illness. This confluence of biological factors explains why the connection between colds and bladder pain is often more pronounced in women than in men.
The Immune System & Bladder Inflammation
A cold initiates an immune response – a cascade of events designed to fight off the viral infection. While essential for recovery, this very process can inadvertently contribute to bladder irritation. When your body detects a virus, it releases cytokines, small proteins that signal inflammation and recruit immune cells to the site of infection (usually the upper respiratory tract). However, these cytokines don’t remain localized; they circulate throughout the bloodstream, potentially reaching other areas of the body, including the urinary tract. This systemic inflammatory response is often overlooked as a cause of bladder discomfort.
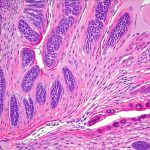
The bladder itself doesn’t have a robust immune system of its own. It relies heavily on the overall immune function and the integrity of surrounding tissues. A compromised or overstimulated immune system (like one battling a cold) can lead to increased bladder sensitivity. This isn’t necessarily an infection, but rather an inflammatory response that mimics UTI symptoms – frequent urination, urgency, pain, and pressure. It’s important to distinguish this from a true bacterial infection, as treatment approaches differ significantly.
The urethra, the tube through which urine exits the body, is also susceptible to inflammation during a cold. Its proximity to the vagina in women increases the risk of irritation, particularly if hygiene practices are altered during illness (e.g., wiping incorrectly). Even mild inflammation can trigger bladder symptoms due to the interconnectedness of these structures and the shared nerve pathways. Recognizing this nuance is vital for accurate diagnosis and effective symptom management.
The Role of Pelvic Floor Dysfunction
Pelvic floor dysfunction (PFD) – a weakening or imbalance of the muscles supporting the pelvic organs – can significantly amplify bladder pain, especially when triggered by illness like a cold. These muscles play a crucial role in urinary control and bladder support. When weakened or tight, they can contribute to bladder irritation and discomfort. A cold can exacerbate PFD in several ways:
- Increased muscle tension: Stress from being sick often leads to increased tension throughout the body, including the pelvic floor muscles. This tightness can put pressure on the bladder and urethra, worsening symptoms.
- Altered movement patterns: When you’re unwell, your movement may change – perhaps adopting a hunched posture or avoiding certain activities. These altered patterns can further strain the pelvic floor muscles.
- Immune response impact: The inflammatory cytokines released during a cold can directly affect nerve function in the pelvic region, increasing sensitivity and pain perception.
Identifying PFD as a contributing factor is essential for comprehensive treatment. Physical therapy specializing in pelvic health can help restore muscle balance and reduce bladder pain. This may involve exercises to strengthen or relax the pelvic floor muscles, as well as techniques to improve posture and movement patterns. It’s important to note that PFD often develops gradually over time and may not be immediately apparent, making it a hidden contributor to chronic bladder pain issues.
Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS) Flare-Ups
For women diagnosed with Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS), even a mild cold can trigger a painful flare-up. IC/BPS is a chronic condition characterized by bladder pain, urinary frequency, and urgency without evidence of infection. The exact cause remains unknown, but it’s believed to involve inflammation, nerve damage, and possibly autoimmune factors.
Colds can exacerbate IC/BPS symptoms through several mechanisms:
– Increased Inflammation: As previously discussed, the systemic inflammatory response triggered by a cold can amplify bladder pain in individuals with IC/BPS, who already have an inflamed bladder lining.
– Immune System Dysregulation: The immune system fluctuations associated with a cold may further disrupt the delicate balance within the bladder and contribute to nerve sensitization.
– Stress & Anxiety: Being sick is inherently stressful, and stress is known to worsen IC/BPS symptoms. This creates a vicious cycle where illness leads to increased pain, which in turn increases stress.
Managing IC/BPS flare-ups requires a multi-faceted approach that includes symptom management strategies like dietary modifications, stress reduction techniques, and potentially medication prescribed by a healthcare professional. It’s crucial for women with IC/BPS to proactively manage their health during cold season and communicate any changes in symptoms to their doctor.
The Gut-Bladder Connection & Microbiome Disruption
Emerging research highlights the close relationship between gut health and bladder function, often referred to as the gut-bladder axis. A healthy gut microbiome – the community of microorganisms living in your digestive tract – plays a vital role in immune regulation and inflammation control. When you get sick with a cold, your immune system shifts focus to fighting off the virus, which can disrupt the delicate balance of your gut microbiome.
This disruption can have several consequences:
– Increased intestinal permeability (“leaky gut”): A compromised gut barrier allows substances like bacterial toxins and undigested food particles to enter the bloodstream, triggering inflammation throughout the body, including the bladder.
– Altered immune function: The gut microbiome profoundly influences immune function. Disruptions can lead to an overactive or imbalanced immune response, contributing to bladder irritation.
– Neurotransmitter imbalances: The gut produces many neurotransmitters that influence mood and pain perception. Changes in the microbiome can affect these levels, potentially exacerbating bladder pain.
Supporting a healthy gut microbiome through dietary changes (e.g., consuming probiotic-rich foods), stress management, and avoiding unnecessary antibiotic use may help reduce bladder pain triggered by colds. This holistic approach recognizes the interconnectedness of body systems and emphasizes proactive health maintenance as a key component of symptom management. Additionally, understanding random bladder pain can provide more insight into these complex connections. It’s also important to consider if tight clothing could be a contributing factor to UTI development. If you suspect a link between your symptoms and illness, it’s helpful to determine if bladder pain is misdiagnosed.
It’s important to remember that this information is for general knowledge and informational purposes only, and does not constitute medical advice. If you are experiencing persistent or severe bladder pain, it’s essential to consult with a healthcare professional for proper diagnosis and treatment. A doctor can accurately assess your condition, rule out other potential causes, and develop an individualized plan to manage your symptoms effectively.