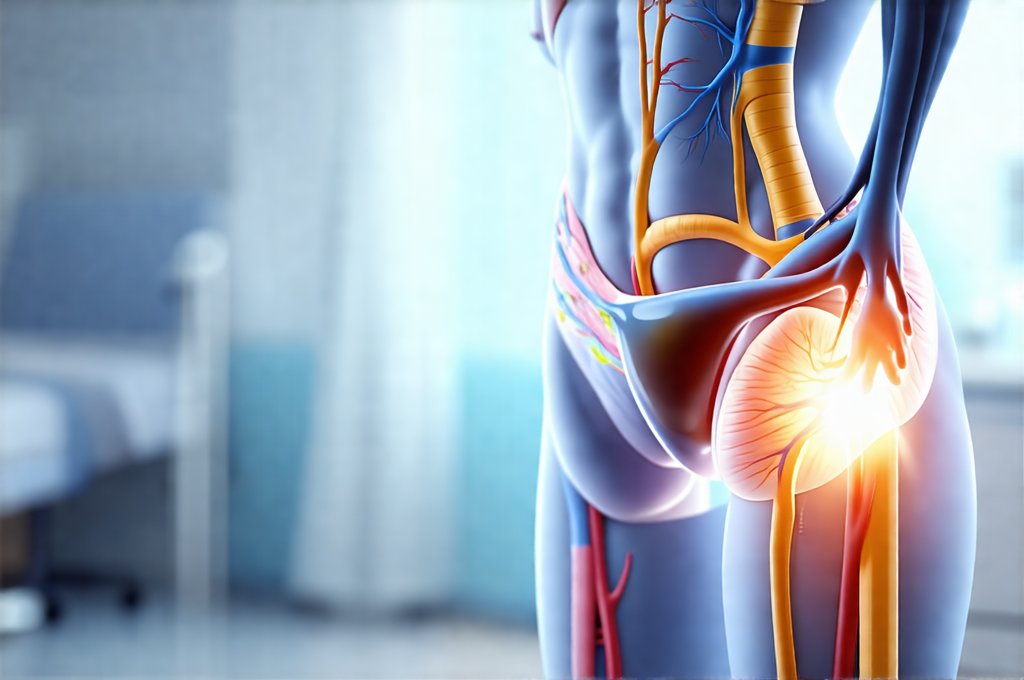
Recurrent cystitis—inflammation of the bladder—is a frustrating condition for many women, often leading to repeated discomfort, disruption to daily life, and anxiety about future flare-ups. Traditional management has frequently involved prolonged courses of antibiotics, which while effective in the short term, can contribute to antibiotic resistance and disrupt the natural microbiome, potentially fueling further infections. Increasingly, research is focusing on the benefits of early intervention and proactive strategies to minimize the severity and frequency of these episodes. This approach shifts the focus from solely treating acute infections to preventing their recurrence, offering a more sustainable and patient-centered solution.
The cornerstone of this evolving understanding lies in recognizing that cystitis isn’t simply an infection, but often a complex interplay between bacterial presence, individual susceptibility (immune response & genetics), bladder function, and lifestyle factors. Early treatment, therefore, doesn’t always mean immediate antibiotics; it encompasses a range of interventions designed to address these underlying issues, reduce inflammation quickly, and prevent the establishment of persistent bacterial colonization. This can involve prompt symptom management, targeted preventative measures, and a tailored approach based on an individual’s history and risk factors, ultimately aiming to break the cycle of recurrent infections before they become deeply entrenched.
Understanding Recurrent Cystitis & The Window of Opportunity
Recurrent cystitis is generally defined as two or more confirmed urinary tract infections (UTIs) within six months, or three or more within a year. However, even less frequent recurrences can significantly impact quality of life. While Escherichia coli (E. coli) is the most common culprit in UTIs, other bacteria and even non-infectious causes like inflammation or bladder hypersensitivity can contribute to symptoms. The key lies in recognizing symptoms early – urgency, frequency, burning sensation during urination, lower abdominal discomfort – and initiating appropriate action swiftly. This “window of opportunity” exists because the bacterial load is typically lowest at the onset of symptoms, making interventions more effective. Delaying treatment allows bacteria to multiply and adhere to the bladder wall, forming biofilms that are significantly harder to eradicate.
The traditional approach often waits for a full-blown infection confirmed by urine culture before initiating antibiotics. However, emerging evidence suggests that even in the early stages, when cultures may be negative or show low bacterial counts, interventions can significantly alter the course of the illness and prevent progression to a symptomatic UTI requiring stronger antibiotic treatment. This is where non-antibiotic strategies play an increasingly vital role. A proactive approach focuses on bolstering the body’s natural defenses and addressing contributing factors before they escalate into established infections.
Furthermore, understanding why recurrences happen is crucial for effective prevention. Factors like hormonal changes (menopause), sexual activity, diaphragm use, genetic predisposition, incomplete bladder emptying, and underlying medical conditions like diabetes can all increase susceptibility. Identifying these individual risk factors allows for targeted preventative strategies. Recognizing early signs is important to help prevent the onset of more severe symptoms.
The Role of Early Intervention Strategies
Early intervention isn’t just about quicker access to antibiotics; it’s about a holistic approach encompassing symptom management, lifestyle modifications, and preventative measures. When symptoms first appear – even before confirming a UTI with a urine culture – increasing fluid intake significantly helps flush bacteria from the urinary tract. Cranberry products (juice or supplements) have been shown in some studies to prevent E. coli adhesion, though evidence is mixed and individual responses vary. D-mannose, a naturally occurring sugar, also works by preventing bacterial adherence. These strategies can often alleviate mild symptoms and potentially avert the need for antibiotics altogether.
However, it’s important to note that self-treating without proper diagnosis isn’t recommended. Consulting a healthcare professional is essential to rule out other conditions and determine the appropriate course of action. If antibiotic treatment is necessary, shorter courses are generally preferred to minimize antibiotic resistance. Low-dose prophylactic antibiotics (taken regularly after intercourse or at specific intervals) can be considered for frequent recurrences, but their use should be carefully evaluated due to potential side effects and the risk of resistance development. A crucial aspect of early intervention is a personalized management plan developed in consultation with a healthcare provider.
Addressing Underlying Risk Factors
Identifying and addressing underlying risk factors is paramount in preventing recurrent cystitis. – Hormonal changes: For postmenopausal women, vaginal estrogen therapy can help restore the protective barrier in the vagina and reduce UTI risk. – Sexual activity: Urinating immediately after intercourse helps flush out bacteria introduced during sexual activity. Avoiding diaphragms or using alternative contraception methods may also be beneficial for some women. – Bladder function: Ensuring complete bladder emptying is crucial. Addressing constipation, which can put pressure on the bladder, is also important. Pelvic floor muscle exercises (Kegels) can strengthen pelvic muscles and improve bladder control.
These lifestyle modifications are often underestimated but play a significant role in long-term prevention. They empower individuals to take control of their health and reduce reliance solely on antibiotics. Furthermore, optimizing overall health through a balanced diet, regular exercise, stress management, and adequate sleep strengthens the immune system and enhances its ability to fight off infections. Maintaining daily activity can also help boost your overall health.
The Importance of Probiotics & Microbiome Health
The gut microbiome – the community of microorganisms living in our digestive tract – is increasingly recognized as playing a vital role in immune function and overall health. Disruptions to the gut microbiome can weaken the immune response, making individuals more susceptible to infections. Similarly, the vaginal microbiome plays a critical role in protecting against UTIs. Antibiotics disrupt both microbiomes, potentially creating an environment conducive to bacterial overgrowth and recurrent infections.
- Probiotic supplementation: Specific probiotic strains, particularly those containing Lactobacillus species, have been shown to help restore a healthy vaginal microbiome and reduce the risk of UTI recurrence. However, it’s crucial to choose probiotics specifically formulated for vaginal health and consult with a healthcare professional before starting supplementation. – Dietary changes: Consuming prebiotic-rich foods (such as onions, garlic, bananas, and oats) can nourish beneficial gut bacteria and promote a healthy microbiome. Avoiding excessive sugar intake and processed foods also supports microbiome balance.
Restoring and maintaining a healthy microbiome is an integral part of a preventative strategy for recurrent cystitis, working in synergy with other interventions to strengthen the body’s natural defenses. Paying attention to early side effects is important when considering microbiome health.
Navigating Long-Term Management & When To Seek Help
Long-term management of recurrent cystitis requires ongoing monitoring and adaptation of treatment plans based on individual responses. Keeping a symptom diary can help identify triggers and patterns, informing preventative strategies. Regular follow-up with a healthcare provider is essential to assess the effectiveness of interventions and adjust them as needed. If symptoms persist despite proactive measures or if new symptoms develop (such as fever, back pain, nausea, or vomiting), it’s crucial to seek immediate medical attention, as these could indicate a more serious infection requiring antibiotic treatment or further investigation.
Ultimately, effective management of recurrent cystitis is a collaborative effort between the individual and their healthcare provider, focusing on early intervention, personalized strategies, and a commitment to long-term health and wellbeing. It’s about shifting from reactive treatment to proactive prevention, empowering individuals to take control of their bladder health and minimize the impact of this frustrating condition on their lives.