Pelvic pain is a complex issue, often shrouded in silence and misunderstanding. Many individuals experiencing chronic pelvic discomfort find themselves navigating a labyrinth of symptoms, diagnoses, and treatments with limited success. A key reason for this difficulty lies in the interconnectedness of the pelvic region – it’s not simply about reproductive organs but encompasses a delicate interplay between muscles, ligaments, nerves, and visceral structures. When these elements aren’t functioning harmoniously, even subtle misalignments can ripple through the system, creating widespread pain and dysfunction. This article will explore how misalignment within the pelvis can specifically contribute to bladder pain, offering insight into potential mechanisms and highlighting the importance of a holistic approach to assessment and treatment.
The experience of bladder pain is often deeply frustrating because it can mimic other conditions—urinary tract infections (UTIs), interstitial cystitis/bladder pain syndrome (IC/BPS), or even gynecological issues. However, frequently overlooked is the role that structural imbalances in the pelvis play in exacerbating these symptoms. It’s crucial to understand that the bladder isn’t an isolated organ; it’s supported and influenced by the surrounding pelvic structures. When these supporting structures are compromised due to misalignment—caused by factors like injury, posture, pregnancy, or repetitive strain – it can directly impact bladder function and sensitivity, leading to chronic discomfort. This is not to suggest that other causes of bladder pain should be dismissed but rather emphasizes a frequently missing piece of the puzzle: structural integrity. If you’re experiencing nighttime discomfort, exploring options like handle nighttime could offer relief.
The Pelvic Floor & Bladder Connection
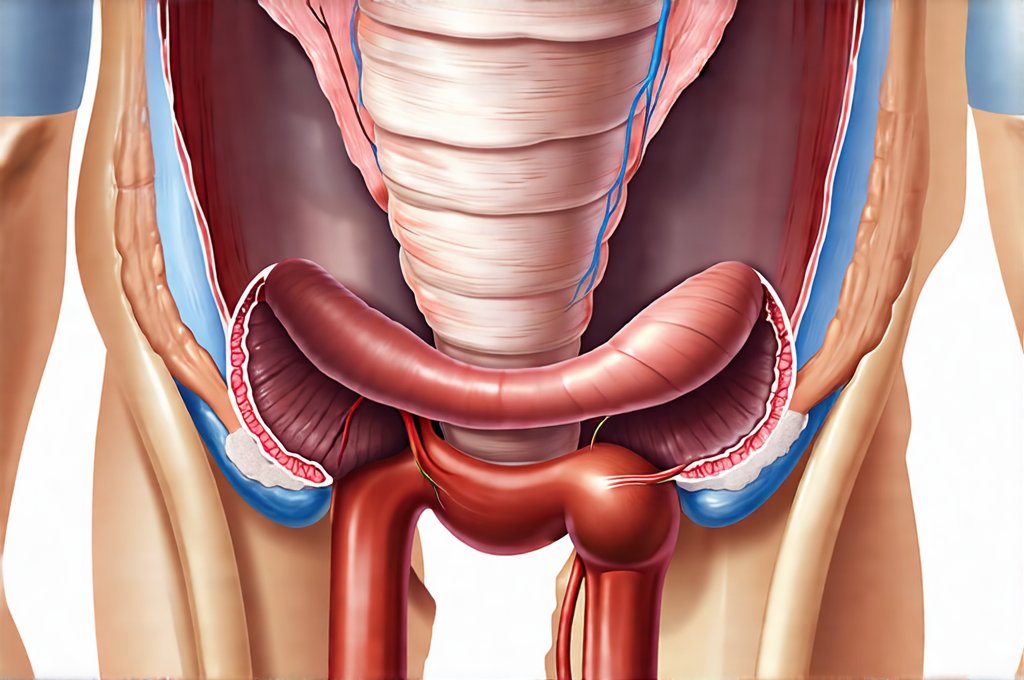
The pelvic floor muscles form a sling-like structure supporting the bladder, uterus (in females), and rectum. They’re essential for urinary and fecal continence, sexual function, and overall pelvic stability. However, when the pelvis is misaligned, it throws off the biomechanics of the pelvic floor. Imagine building a house on an uneven foundation – everything above will be unstable. Similarly, a misaligned pelvis can cause one side of the pelvic floor to become overactive and tight while the other side weakens. This imbalance not only affects bladder control but also compresses nerves and blood vessels in the area, contributing directly to pain signals. – Tight pelvic floor muscles restrict blood flow and lymphatic drainage, creating inflammation and increased sensitivity within the bladder wall. – A weakened pelvic floor can lead to bladder prolapse or instability, causing urgency and frequency. – Nerve compression from muscle imbalances can mimic IC/BPS symptoms, leading to misdiagnosis.
Furthermore, the alignment of the sacrum—the triangular bone at the base of the spine that connects to the pelvis – is critical. Sacral dysfunction, a common result of pelvic misalignment, directly impacts the nerves exiting the sacrum which innervate the bladder and surrounding structures. – A forward or backward tilt of the sacrum can put pressure on these nerves, leading to altered bladder sensation and pain. – Restrictions in sacral motion limit the ability of the pelvic floor muscles to function optimally, further contributing to dysfunction. – Addressing sacral alignment is often a key component of successful treatment for chronic bladder pain. Understanding intermittent bladder onset can help you proactively manage discomfort.
Contributing Factors & Structural Imbalance
Several factors can contribute to pelvic misalignment, creating the conditions for bladder pain to develop. Posture plays a significant role; prolonged sitting, poor ergonomic setup at work, and habitual slouching can all create imbalances over time. – Repetitive movements or activities like running or cycling, without proper core support, can strain the pelvic structures. – Injuries such as falls, car accidents, or childbirth (even without complications) can disrupt the natural alignment of the pelvis. – Pre-existing conditions like scoliosis or leg length discrepancies also impact pelvic stability and contribute to imbalances.
Hormonal changes, particularly during pregnancy and menopause, affect ligament laxity, making the pelvis more vulnerable to misalignment. – Pregnancy significantly alters biomechanics due to weight gain and shifts in center of gravity; appropriate support and rehabilitation are crucial. – Menopause leads to decreased estrogen levels, which weakens ligaments and connective tissues, increasing pelvic instability. It’s important to note that these factors often don’t act in isolation but rather combine to create a complex interplay contributing to structural imbalances and subsequent bladder pain. Identifying the root causes of misalignment is essential for developing an effective treatment plan. Birth can lead to long-term changes in pelvic health, making it important to be aware of potential issues.
Assessing Pelvic Alignment & Function
Accurate assessment is paramount in understanding the underlying mechanisms driving bladder pain. A comprehensive evaluation should go beyond standard urological tests and incorporate several key components: – Physical examination: This includes assessing posture, gait, spinal alignment, sacral motion, pelvic floor muscle function (tone, strength, coordination), and palpating for areas of tenderness or restriction. – Movement assessment: Evaluating how the pelvis moves during functional tasks like walking, squatting, and bending helps identify imbalances and limitations. – Neurological screening: Assessing nerve function to rule out nerve compression or entrapment contributing to pain.
Specialized techniques like Real-Time Ultrasound (RTUS) can provide valuable insights into pelvic floor muscle function in real time, allowing clinicians to assess coordination and identify areas of weakness or overactivity. It’s also important to take a detailed history including information about previous injuries, surgeries, lifestyle factors, and pain patterns. A collaborative approach between healthcare professionals – physical therapists specializing in pelvic health, urologists, gynecologists, and pain management specialists – is often the most effective way to ensure a thorough evaluation and tailored treatment plan.
Restoring Pelvic Balance: Treatment Approaches
Treatment for bladder pain related to pelvic misalignment focuses on restoring structural balance, improving pelvic floor function, and reducing nerve compression. – Manual therapy: Techniques like myofascial release, joint mobilization, and muscle energy techniques can address restrictions in the sacrum, pelvis, and surrounding tissues, releasing tension and restoring proper alignment. – Pelvic floor rehabilitation: This includes exercises to strengthen weak muscles, relax overactive muscles, and improve coordination. Biofeedback and electrical stimulation may be used to enhance awareness and facilitate correct movement patterns.
- Postural correction & ergonomic advice: Addressing postural habits and providing guidance on proper body mechanics can prevent recurrence of imbalances. – Pain management strategies: Techniques like trigger point therapy, dry needling, or gentle stretching can help alleviate pain and improve function. It’s crucial to remember that treatment is often individualized and may require a combination of these approaches. Furthermore, addressing underlying factors such as stress, anxiety, or emotional trauma – which can contribute to pelvic floor tension – is vital for long-term success. A holistic approach that considers the physical, emotional, and psychological aspects of pain will yield the most positive outcomes. If you’re experiencing radiating discomfort, learning about bladder pain radiate can help understand your symptoms better.