Neuroinflammation, once considered solely a phenomenon within the central nervous system, is now increasingly recognized as a key player in a wide range of systemic conditions – including those affecting seemingly distant organs like the bladder. The intricate interplay between the brain, immune system and peripheral tissues means that inflammation originating or exacerbated by neurological processes can have far-reaching consequences for overall health. This emerging understanding challenges traditional views of disease pathogenesis and opens new avenues for therapeutic intervention, focusing not just on local treatment but also on addressing underlying neuroinflammatory drivers. Understanding this connection is vital as chronic bladder conditions are often difficult to manage, with many patients experiencing persistent symptoms despite conventional therapies.
The link between neuroinflammation and bladder health isn’t about a direct anatomical connection, like nerves directly inflaming the bladder wall – though that can happen in specific cases. It’s more subtle, stemming from the brain’s influence on immune regulation, pain processing, and visceral function. The nervous system acts as a central command center, modulating inflammatory responses throughout the body. When neuroinflammation disrupts this regulatory capacity, it can lead to chronic inflammation in peripheral organs like the bladder, even without a clear localized cause. Furthermore, altered pain pathways due to neuroinflammation can amplify the perception of bladder discomfort and contribute to conditions like interstitial cystitis/bladder pain syndrome (IC/BPS). This is particularly relevant as IC/BPS often presents with symptoms disproportionate to any visible inflammation within the bladder itself, suggesting a significant role for central sensitization. Understanding the link between estrogen and bladder health can also shed light on these connections.
The Brain-Bladder Axis: A Two-Way Street
The relationship between the brain and bladder isn’t unidirectional; it’s a complex bidirectional communication system known as the brain-bladder axis. This axis involves neural pathways, hormonal signals, and immune mediators that constantly exchange information between the two organs. The brain influences bladder function through autonomic nervous system control – dictating storage capacity, micturition reflexes, and pain perception. Conversely, the bladder sends sensory information back to the brain, informing it about fullness, discomfort, or inflammation. Neuroinflammation can disrupt this delicate balance in several ways. For example, chronic stress and associated neuroinflammation can lead to increased sympathetic nervous system activity, contributing to bladder overactivity and urgency. Similarly, inflammatory cytokines released during neuroinflammation can alter pain thresholds within the brain, making individuals more sensitive to bladder-related discomfort. What’s the difference between continuous and intermittent flow is also important when assessing bladder function.
The gut microbiome also plays a vital role in this axis, acting as an intermediary between the brain and bladder. Gut dysbiosis, often linked to neuroinflammation, can increase intestinal permeability (“leaky gut”), allowing inflammatory molecules to enter the bloodstream and trigger systemic inflammation – including within the bladder. This highlights the importance of considering the gut microbiome when evaluating and managing chronic bladder conditions. A healthy gut microbiome promotes a balanced immune response and reduces the risk of neuroinflammation, ultimately supporting optimal bladder health. Furthermore, emerging research suggests that specific probiotic strains may help modulate both the gut microbiome and brain function, offering a novel therapeutic approach for individuals with IC/BPS or other bladder disorders.
Neuroinflammation & Common Bladder Conditions
Neuroinflammation is increasingly implicated in the pathogenesis of several common bladder conditions. In Overactive Bladder (OAB), for instance, neuroinflammation may contribute to altered detrusor muscle function and increased urgency-frequency syndrome. Chronic pelvic pain syndromes, including IC/BPS, are particularly linked to neuroinflammation, with studies showing elevated levels of inflammatory markers in the brains of affected individuals. The persistent pain associated with these conditions can itself exacerbate neuroinflammation, creating a vicious cycle. Even seemingly straightforward issues like stress incontinence may be influenced by neuroinflammation, as it can impair the brain’s ability to effectively control pelvic floor muscles and urethral sphincter function.
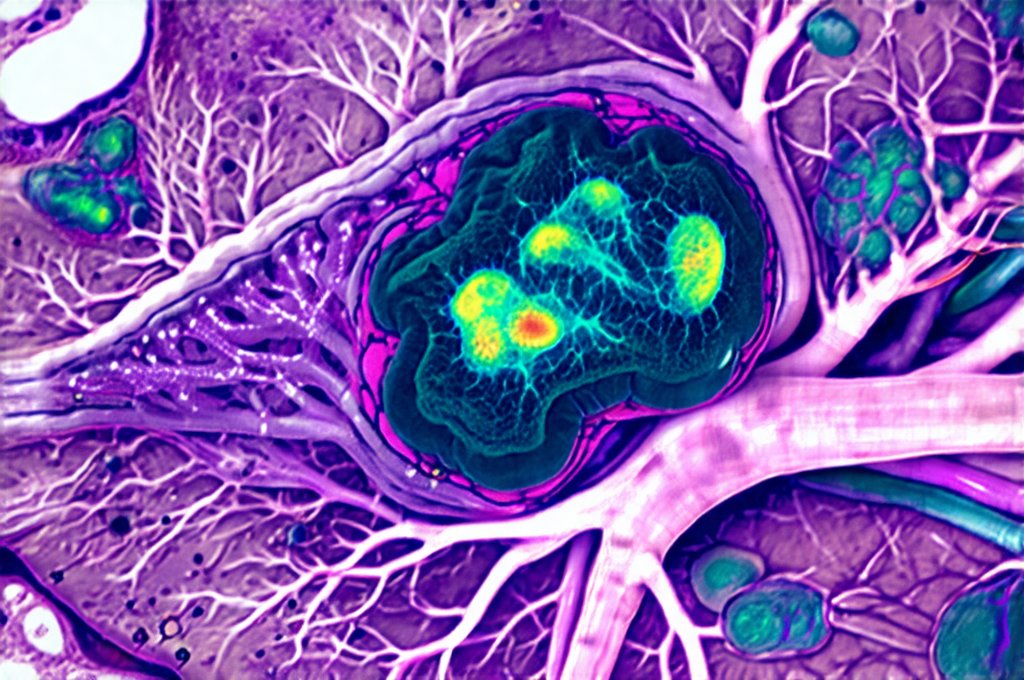
The role of glial activation in neuroinflammation is particularly noteworthy. Glial cells, including microglia and astrocytes, are immune cells within the central nervous system. When activated chronically due to stress, infection or trauma, they release pro-inflammatory cytokines that contribute to neuronal dysfunction and pain sensitization. This glial activation isn’t just a consequence of bladder problems; it can precede them, setting the stage for chronic symptoms. Addressing neuroinflammation therefore requires a holistic approach targeting not only the peripheral bladder but also the central nervous system and underlying inflammatory drivers.
Identifying Neuroinflammatory Contributions
Determining whether neuroinflammation is playing a role in an individual’s bladder health can be challenging, as there isn’t one single diagnostic test. However, several clinical clues should raise suspicion:
- Persistent symptoms despite conventional treatment: If standard therapies for OAB or IC/BPS fail to provide adequate relief, it suggests that underlying factors beyond localized inflammation may be at play.
- Co-morbid conditions: The presence of other neuroinflammatory conditions – such as fibromyalgia, chronic fatigue syndrome, or depression – increases the likelihood of a neuroinflammatory component in bladder symptoms.
- History of trauma or stress: Individuals with a history of chronic stress, adverse childhood experiences, or traumatic events are more vulnerable to neuroinflammation and its associated health consequences.
- Gut health issues: Symptoms of gut dysbiosis, such as bloating, diarrhea, or constipation, suggest a potential link between the gut microbiome and bladder dysfunction.
While imaging techniques like functional MRI (fMRI) can assess brain activity and identify areas of inflammation, they are not routinely used for diagnosing neuroinflammation in relation to bladder health. Biomarker testing – measuring inflammatory markers in blood or cerebrospinal fluid – is still evolving but may offer a more objective way to assess neuroinflammatory status in the future. A comprehensive assessment including detailed patient history, physical examination, and potentially some specialized testing can help identify individuals who might benefit from interventions targeting neuroinflammation.
Therapeutic Strategies for Neuroinflammation & Bladder Health
Addressing neuroinflammation requires a multi-faceted approach that goes beyond traditional bladder treatments. Lifestyle modifications are often the first line of defense:
- Stress management: Techniques like mindfulness, meditation, yoga, and deep breathing exercises can help reduce stress and mitigate neuroinflammatory responses.
- Dietary changes: An anti-inflammatory diet rich in omega-3 fatty acids, antioxidants, and fiber can support gut health and reduce systemic inflammation. Reducing processed foods, sugar, and inflammatory fats is also crucial.
- Regular exercise: Physical activity promotes the release of endorphins – natural mood boosters that also have anti-inflammatory effects.
Beyond lifestyle changes, several targeted therapies may be beneficial:
- Nutritional supplements: Certain supplements, such as curcumin (from turmeric), omega-3 fatty acids, and probiotics, have demonstrated anti-inflammatory properties and may help modulate neuroinflammation.
- Neuromodulation techniques: Transcranial magnetic stimulation (TMS) and vagus nerve stimulation (VNS) are non-invasive therapies that can influence brain activity and potentially reduce pain sensitization in IC/BPS patients.
- Low dose naltrexone (LDN): This medication, originally used for opioid addiction, has shown promise in reducing neuroinflammation and alleviating chronic pain in various conditions, including fibromyalgia and potentially IC/BPS.
Future Directions & Research Needs
The connection between neuroinflammation and bladder health is a relatively new area of research, and much remains to be understood. Future studies are needed to: identify specific biomarkers that can accurately assess neuroinflammatory status; elucidate the precise mechanisms by which neuroinflammation contributes to different bladder conditions; and develop targeted therapies specifically designed to address neuroinflammation in relation to bladder dysfunction. Furthermore, investigating the role of the gut microbiome and its influence on the brain-bladder axis is crucial for developing novel preventative and therapeutic strategies. As our understanding of this complex interplay continues to evolve, we can expect to see more effective and personalized approaches to managing chronic bladder conditions – moving beyond symptom management towards addressing the underlying inflammatory drivers that contribute to these debilitating disorders. What’s the link between IBS and UTIs in women? is a question increasingly being researched alongside these connections.