Cystitis, an inflammation of the bladder, is a remarkably common ailment, particularly affecting women. Many experience it as intensely uncomfortable – a burning sensation during urination, frequent urges to go, and a general feeling of pressure in the pelvic area. While antibiotics are often effective at clearing up the acute infection, a frustratingly large number of individuals find themselves battling recurring episodes. This isn’t simply about a persistent infection; it’s frequently indicative of underlying factors that remain unaddressed after initial treatment, creating a cycle of symptoms and antibiotic use. Understanding why cystitis returns is crucial to breaking this cycle and achieving long-term relief.
The common approach of relying solely on antibiotics for each flare-up can actually contribute to the problem in several ways. Repeated antibiotic courses disrupt the natural microbiome – both within the gut and, importantly, within the urinary tract itself – potentially making individuals more susceptible to future infections. Furthermore, some bacteria can develop resistance to commonly used antibiotics over time, reducing their effectiveness. It’s important to recognize that cystitis isn’t always a straightforward bacterial infection; it can be linked to various factors including hormonal changes, anatomical predispositions, and even lifestyle choices which often go unnoticed. A holistic understanding of these contributing elements is essential for effective management.
Understanding Recurring Cystitis: Beyond the Bacteria
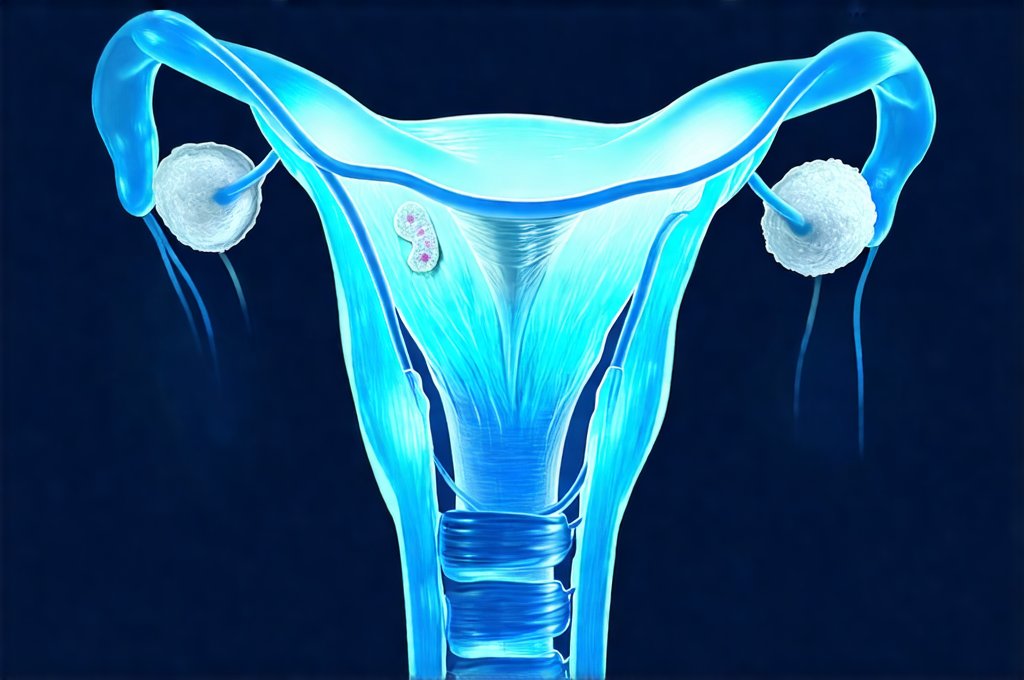
The conventional view of cystitis focuses heavily on Escherichia coli (E. coli) as the primary culprit – and it indeed is responsible for a significant percentage of cases. However, to assume that every recurrence is simply a re-infection with E. coli overlooks the complexity of the urinary tract and the body’s defense mechanisms. Recurring cystitis can often be attributed to factors that weaken these defenses, making the bladder more vulnerable to bacterial adherence and colonization. These factors include anatomical variations – such as a shorter urethra in women increasing ease of access for bacteria – hormonal fluctuations during menopause or pregnancy, and conditions like diabetes which compromise immune function.
Moreover, the urinary microbiome—the community of microorganisms inhabiting the urinary tract—is increasingly recognized as playing a vital role in preventing infections. A healthy urinary microbiome acts as a barrier against pathogenic bacteria, competing for resources and producing antimicrobial substances. Antibiotic use can disrupt this delicate balance, creating an environment where harmful bacteria can thrive. This disruption isn’t always immediately apparent but can significantly impact long-term susceptibility to infection. It’s also important to consider non-bacterial causes of cystitis symptoms, such as interstitial cystitis (painful bladder syndrome), which requires a different approach to treatment and management. If you are experiencing recurring issues, it may be time to understand why UTIs keep coming back after treatment.
Finally, behavioral factors play a role. Insufficient hydration, infrequent voiding, and poor hygiene practices can all contribute to bacterial build-up in the urinary tract and increase the risk of infection. Recognizing these often-overlooked aspects is key to developing a comprehensive strategy for preventing recurrence.
The Role of Hormonal Changes & Immune Function
Hormonal shifts, particularly those experienced during menopause, are strongly linked to increased susceptibility to recurrent cystitis. As estrogen levels decline, the vaginal and urinary tract tissues become thinner and drier, reducing their natural protective barrier against bacteria. This creates a more alkaline environment in the vagina, which favors E. coli growth. Hormone replacement therapy (HRT), when appropriate and prescribed by a healthcare professional, can help restore estrogen levels and improve the health of these tissues. However, HRT isn’t suitable for everyone and requires careful evaluation of individual risks and benefits.
Beyond hormones, a compromised immune system is a significant factor in recurring cystitis. Conditions like diabetes, autoimmune diseases, or even chronic stress can weaken the body’s ability to fight off infection. A robust immune system relies on adequate nutrition, sleep, and regular exercise. Supporting immune function through lifestyle modifications – such as consuming a balanced diet rich in vitamins and minerals, getting sufficient rest, and managing stress levels—can significantly reduce the risk of recurrence. It’s also important to note that gut health is intimately connected to immune function; a healthy gut microbiome contributes to a stronger immune response.
It’s vital to differentiate between recurrent infection and persistent inflammation. Sometimes, even after successful antibiotic treatment, low-grade inflammation can remain in the bladder lining, contributing to ongoing symptoms and increasing vulnerability to future infections. This is where addressing underlying factors becomes paramount.
Identifying & Addressing Underlying Factors
Many individuals experiencing recurring cystitis haven’t fully investigated the root causes beyond the initial infection. A thorough medical evaluation is crucial to identify any contributing factors that may be present. This includes:
- Urological assessment: To rule out anatomical abnormalities or other urological conditions.
- Hormonal evaluation: Particularly for postmenopausal women, to assess estrogen levels and consider HRT if appropriate.
- Immune function testing: In some cases, evaluating immune markers may help identify underlying immune deficiencies.
- Dietary & Lifestyle review: A detailed look at hydration habits, dietary choices, stress management techniques, and hygiene practices.
Once potential contributing factors are identified, a tailored management plan can be developed. If you find yourself in this situation, knowing how long after treatment should UTI pain stop is vital to understanding your recovery process.
Prevention Strategies for Reducing Recurrence
Preventing cystitis recurrence often involves a multifaceted approach focusing on lifestyle modifications and proactive measures. Here’s a breakdown of effective strategies:
- Hydration: Drinking plenty of water – typically 6-8 glasses per day – helps to flush bacteria out of the urinary tract.
- Frequent Voiding: Avoid holding urine for extended periods; empty your bladder regularly, especially after sexual activity.
- Post-Coital Voiding: Urinating immediately after intercourse can help eliminate any bacteria that may have entered the urethra during sexual activity.
- Dietary Modifications: Reducing intake of caffeine, alcohol, and spicy foods may help soothe an irritated bladder. Some individuals find relief by avoiding acidic foods like citrus fruits or tomatoes, although this varies greatly from person to person.
- Probiotics: Supplementing with probiotics – specifically those containing strains known to support urinary tract health—can help restore a healthy vaginal and urinary microbiome. Lactobacillus species are often recommended.
- D-Mannose: This naturally occurring sugar can prevent E. coli from adhering to the bladder wall, reducing the risk of infection. It’s available as a dietary supplement.
Exploring Alternative Therapies & Long-Term Management
While antibiotics remain a mainstay in treating acute cystitis infections, alternative therapies and long-term management strategies can play a vital role in preventing recurrence. These include:
- Cranberry Products: Although research is mixed, some studies suggest that cranberry products (juice or supplements) may help prevent E. coli from adhering to the bladder wall. However, it’s important to be aware of potential drug interactions and sugar content.
- Herbal Remedies: Certain herbal remedies, such as uva ursi and buchu leaf, have traditionally been used for urinary tract health. However, these should only be used under the guidance of a qualified healthcare professional due to potential side effects and interactions with medications.
- Pelvic Floor Exercises: Strengthening the pelvic floor muscles can improve bladder control and reduce the risk of urinary leakage, which can contribute to infection.
- Mindful Bladder Habits: Learning to recognize genuine urges to urinate versus habit-based voiding can help avoid overactive bladder symptoms and promote healthy bladder function.
Long-term management requires a collaborative approach between patient and healthcare provider. Regular follow-up appointments, ongoing monitoring of symptoms, and adjustments to the management plan as needed are essential for achieving lasting relief from recurring cystitis. It’s also critical to remember that self-treating with antibiotics is strongly discouraged, as it can contribute to antibiotic resistance and mask underlying issues. If you’re concerned about experiencing these challenges again, understanding why UTIs return after treatment in women can provide valuable insight.