Immune dysfunction plays a complex role in many chronic illnesses, and increasingly, research is pointing towards intricate connections between seemingly disparate conditions. Endometriosis, a painful condition where tissue similar to the lining of the uterus grows outside of it, and Immune Cell (IC) dysregulation – specifically abnormalities in how various immune cells function – are two such areas now under intense scrutiny. For years, endometriosis was primarily understood as a gynecological disorder; however, its systemic effects and potential link to broader immunological issues are becoming increasingly apparent. Understanding these connections is crucial for developing more effective diagnostic tools and therapeutic strategies that address the root causes of this debilitating condition rather than just managing symptoms.
The emerging evidence suggests that ICs aren’t merely responding to endometriosis but may actually be involved in its development, progression, and chronic pain aspects. This isn’t a simple case of an overactive or underactive immune system; it’s far more nuanced. Specific types of ICs exhibit altered behavior in individuals with endometriosis, creating a complex inflammatory environment that perpetuates the disease. Researchers are now focusing on identifying these specific immunological signatures to improve early detection and develop targeted therapies aimed at modulating the immune response. This shift in perspective is revolutionizing how we approach understanding and treating this often-misunderstood condition.
The Immunological Landscape of Endometriosis
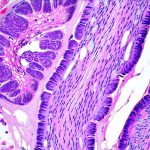
Endometriosis isn’t simply about misplaced tissue; it’s fundamentally an immunological disease, or at least heavily influenced by immunological processes. Traditionally, the immune system should recognize ectopic endometrial tissue as “non-self” and eliminate it. However, in endometriosis, this recognition and clearance process are often impaired, leading to the establishment of lesions. Several factors contribute to this impairment, including defects in natural killer (NK) cell function, altered cytokine profiles, and the presence of regulatory T cells (Tregs). NK cells, critical for identifying and destroying abnormal cells, have been shown to be less active in women with endometriosis. This reduced activity allows endometrial implants to evade immune surveillance and persist.
Cytokines – signaling molecules that mediate immune responses – are also dysregulated in endometriosis. While some pro-inflammatory cytokines (like TNF-alpha and IL-6) are elevated, contributing to pain and inflammation, others that promote immune tolerance may also be present, further complicating the picture. This complex cytokine milieu creates a microenvironment that fosters lesion growth and perpetuates chronic inflammation. The role of Tregs is particularly interesting; these cells normally suppress immune responses to prevent autoimmunity, but in endometriosis, they seem to be recruited to lesions, contributing to local immunosuppression and allowing implants to thrive.
Furthermore, the composition of the gut microbiome can profoundly impact the immune system, and alterations in gut bacteria have been linked to endometriosis. A disrupted microbiome (dysbiosis) can lead to increased intestinal permeability (“leaky gut”), allowing bacterial products to enter the bloodstream and trigger systemic inflammation, potentially exacerbating endometrial lesions. This highlights the importance of considering a holistic approach to treatment that addresses both local and systemic immunological factors.
Immune Cell Specifics in Endometriosis
The involvement of various IC types is critical to understanding the pathogenesis of endometriosis. Macrophages, versatile immune cells involved in phagocytosis (engulfing and destroying pathogens) and tissue repair, play a dual role. Initially, they attempt to clear ectopic endometrial tissue; however, over time, they can become “M2-polarized,” meaning they shift from a pro-inflammatory state to one that promotes tissue remodeling and angiogenesis (formation of new blood vessels), thereby supporting lesion growth.
Similarly, dendritic cells – antigen-presenting cells that initiate immune responses – exhibit altered function in endometriosis. They may fail to effectively present endometrial antigens to T cells, leading to impaired T cell activation and a reduced ability to clear lesions. B cells also play a role, with some studies suggesting that autoantibodies against endometrial tissue contribute to inflammation and disease progression. In essence, the interplay between these different ICs creates a dysregulated immune environment where endometrial implants are able to survive and proliferate despite being recognized as foreign by the body’s defense mechanisms. The specific subtypes of each cell involved and their interactions are still under investigation but represent a rapidly evolving area of research.
Identifying Immune Biomarkers for Early Detection
One of the most promising avenues in endometriosis research is identifying reliable immune biomarkers that can aid in early detection and diagnosis. Currently, diagnosis relies heavily on laparoscopic surgery, which is invasive and often delayed due to vague or non-specific symptoms. – Researchers are exploring several potential biomarkers, including levels of specific cytokines (e.g., IL-6, TNF-alpha) in blood or peritoneal fluid, the number and activity of NK cells, and the presence of autoantibodies against endometrial tissue.
- Another promising approach is analyzing immune cell populations within lesions themselves through biopsies. This allows for a more detailed assessment of the local immunological environment and can help identify specific immune signatures associated with different stages of disease severity. – Machine learning algorithms are also being used to analyze complex datasets from multiple sources (e.g., genomics, proteomics, metabolomics) to identify novel biomarkers that may not be apparent through traditional methods.
The development of non-invasive diagnostic tests based on these biomarkers would revolutionize endometriosis care, leading to earlier diagnosis, reduced delays in treatment, and improved patient outcomes. However, it’s important to note that identifying reliable biomarkers is challenging due to the heterogeneity of the disease and individual variations in immune responses.
The Gut-Immune Connection & Endometriosis
The gut microbiome – the trillions of bacteria residing in our intestines – plays a vital role in shaping the immune system. Disruptions in this microbial ecosystem (dysbiosis) have been increasingly linked to various autoimmune and inflammatory diseases, including endometriosis. A compromised gut barrier can lead to “leaky gut,” allowing bacterial products like lipopolysaccharide (LPS) to enter the bloodstream and trigger systemic inflammation.
This chronic low-grade inflammation can exacerbate endometrial lesions and contribute to pain symptoms. Specific microbial imbalances have been observed in women with endometriosis compared to healthy controls, suggesting a potential causal relationship. – Dietary interventions aimed at restoring gut health, such as increasing fiber intake, reducing processed foods, and incorporating probiotic supplements, may help modulate the immune response and alleviate endometriosis symptoms.
- Fecal Microbiota Transplantation (FMT), which involves transferring fecal matter from a healthy donor to a recipient, is being investigated as a potential therapeutic strategy for restoring gut microbial balance and improving immunological function in women with endometriosis. However, more research is needed to determine the safety and efficacy of FMT for this condition. The complex interplay between the gut microbiome and the immune system highlights the importance of considering a holistic approach to treatment that addresses both local and systemic factors.
Immunomodulatory Therapies: Future Directions
Traditional treatments for endometriosis often focus on hormonal therapy or surgical removal of lesions, but these approaches don’t address the underlying immunological dysfunction. Immunomodulatory therapies – treatments aimed at regulating the immune system – are emerging as promising alternatives. – One approach is using biologics, such as monoclonal antibodies, to target specific cytokines or immune cells involved in endometriosis pathogenesis. For example, anti-TNF-alpha therapy has shown some promise in reducing inflammation and pain symptoms in certain patients.
- Another strategy is using immunopeptides – small fragments of proteins that can modulate immune responses. These peptides can be designed to either enhance immune clearance of ectopic endometrial tissue or suppress local inflammation. – Emerging therapies like CAR T-cell therapy, which involves genetically engineering a patient’s own T cells to target and destroy specific cells, are also being explored as potential treatments for endometriosis. However, these therapies are still in early stages of development and require further research to ensure their safety and efficacy.
The challenge lies in developing immunomodulatory strategies that selectively target the dysregulated immune responses without causing unwanted side effects or compromising overall immune function. Precision medicine approaches, tailoring treatment based on individual immunological profiles, will be crucial for maximizing therapeutic benefits and minimizing risks.