Bladder pain syndrome (BPS) and interstitial cystitis (IC) are terms often used interchangeably, leading to confusion for patients and healthcare professionals alike. Both conditions describe chronic pelvic pain believed to originate from the bladder, but their understanding has evolved significantly over time. Historically, IC was considered a specific diagnosis characterized by unique histological findings in the bladder lining – specifically, mast cell activation and glomerulations (small pinpoint hemorrhages). However, as research advanced, it became clear that many individuals presenting with these symptoms did not exhibit those characteristics, suggesting a broader spectrum of conditions causing similar pain. This led to the development of BPS as an umbrella term encompassing all chronic bladder pain presentations, regardless of the presence or absence of the “classic” IC features.
The core issue is that the diagnostic criteria and understanding of these conditions have undergone significant changes, resulting in overlapping definitions and a lack of consensus. While some clinicians still adhere to the traditional definition of IC requiring specific histological findings, many now favor a symptom-based diagnosis focusing on the severity and impact of pelvic pain, urinary frequency, and urgency—characteristics common to both BPS and IC. This shift has blurred the lines between the two conditions, making it difficult to determine whether they are distinct entities or different manifestations of the same underlying problem. Ultimately, the terminology used often depends on the individual physician’s approach and understanding, leading to inconsistencies in diagnosis and treatment. Many patients wonder is interstitial cystitis the same as prostatitis?.
The Evolution of Diagnostic Criteria
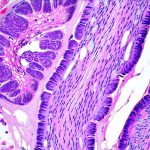
The initial description of interstitial cystitis, dating back to the 19th century, focused heavily on ulcerations observed during bladder examinations. However, this “ulcerative” IC was later found to be relatively rare. In the mid-20th century, Dr. György Lettenmaier introduced the concept of “interstitial cystitis” as we initially understood it – identifying glomerulations and mast cell activation as key diagnostic markers during cystoscopy (a procedure involving bladder visualization). This became the gold standard for diagnosis, but also limited its application, as many patients with chronic bladder pain didn’t fit this profile. The 1987 National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) consensus criteria attempted to address this by broadening the diagnostic parameters, incorporating symptom severity and duration alongside cystoscopic findings.
The problem remained that even with the NIDDK criteria, a significant number of patients presented with chronic bladder pain but lacked the characteristic cystoscopic features. This led to the coining of “bladder pain syndrome” (BPS) in 1990s, as a more inclusive term for all chronic bladder pain conditions. BPS acknowledged that chronic pelvic pain could arise from multiple factors beyond just inflammation or ulceration within the bladder wall itself. Modern diagnostic approaches are increasingly focusing on a comprehensive assessment of symptoms and ruling out other potential causes, rather than relying solely on cystoscopic findings. This symptom-based approach recognizes the heterogeneity of these conditions and aims to tailor treatment based on individual patient needs. Some people experience sharp stabbing pain when the bladder is empty.
Understanding the Overlap and Differences
Despite the evolution in terminology, it’s essential to understand where the overlap and subtle differences lie. IC, in its traditional definition, is often associated with more pronounced bladder wall changes – like inflammation or scarring – observed during cystoscopy. It frequently presents with significant urinary urgency and frequency, sometimes accompanied by pain that worsens with bladder filling. BPS, on the other hand, is a broader category encompassing patients who experience chronic pelvic pain but may have minimal to no visible abnormalities during cystoscopy. They might still report similar symptoms of frequency and urgency, but the intensity can vary considerably.
Crucially, both conditions are often associated with comorbid conditions – meaning they frequently occur alongside other health issues. These can include irritable bowel syndrome (IBS), fibromyalgia, vulvodynia, and chronic fatigue syndrome, suggesting a potential link between pelvic pain syndromes more broadly. The underlying causes of BPS and IC remain largely unknown, adding to the complexity. Current research points towards multiple factors potentially contributing to these conditions including nerve dysfunction, immune system abnormalities, and genetic predisposition. It’s important to note that some patients may initially be diagnosed with one condition only to have their diagnosis change as more information becomes available or symptoms evolve over time.
Diagnostic Challenges and Approaches
Diagnosing BPS/IC can be a challenging process due to the subjective nature of symptoms and the lack of definitive biomarkers. Unlike many other conditions, there isn’t a single test that can definitively confirm the diagnosis. The diagnostic process typically involves a thorough medical history, physical examination (including pelvic exam), urine analysis to rule out infection or other causes, and potentially cystoscopy. However, as previously mentioned, cystoscopic findings are not always present or conclusive.
- Symptom questionnaires: Tools like the Pelvic Pain, Urgency, and Frequency (PUF) questionnaire help quantify symptom severity and track changes over time.
- Potassium chloride sensitivity test: This involves instilling potassium chloride solution into the bladder to assess for pain response, potentially indicating heightened nerve sensitivity.
- Bladder diary: Tracking urination frequency, urgency, and associated pain can provide valuable information about symptom patterns.
A key aspect of diagnosis is ruling out other potential causes of pelvic pain, such as urinary tract infections, kidney stones, sexually transmitted infections, endometriosis (in women), and prostate problems (in men). A multidisciplinary approach involving urologists, gynecologists, gastroenterologists, and pain specialists can be beneficial to ensure a comprehensive evaluation. It’s important to distinguish is a cyst the same as a tumor?.
The Role of Nerve Dysfunction in BPS/IC
Growing evidence suggests that nerve dysfunction plays a significant role in the development and perpetuation of BPS/IC symptoms. This is often referred to as “neuropathic bladder pain.” Damaged or hypersensitive nerves in the bladder wall can amplify pain signals, leading to chronic pelvic discomfort even in the absence of obvious inflammation. Several factors can contribute to nerve dysfunction, including:
- Inflammation: While traditional IC focused on mast cell activation, subtle inflammatory processes might still play a role in triggering nerve sensitization.
- Microtrauma: Repeated bladder filling and emptying or sexual activity could potentially cause microtrauma to the bladder lining, damaging nerve fibers over time.
- Central sensitization: Chronic pain can lead to changes in the central nervous system (brain and spinal cord), amplifying pain signals and reducing pain thresholds.
Treatments aimed at addressing nerve dysfunction – such as neuromodulation therapy (sacral nerve stimulation or posterior tibial nerve stimulation) – have shown promise in some patients, highlighting the importance of this pathway in understanding BPS/IC. Additionally, medications targeting neuropathic pain, like amitriptyline or gabapentin, may be used to manage symptoms.
Current and Emerging Treatments
Treatment for BPS/IC is often multimodal, meaning it involves a combination of approaches tailored to the individual patient’s symptoms and needs. There’s no “one-size-fits-all” solution, as what works for one person might not work for another. Common treatment options include:
- Lifestyle modifications: Avoiding bladder irritants (caffeine, alcohol, acidic foods), managing stress, and practicing pelvic floor muscle relaxation techniques can help reduce symptoms.
- Medications: Pentosan polysulfate sodium (Elmiron) is a medication specifically approved for IC, although its efficacy remains debated. Other medications used to manage symptoms include pain relievers, antispasmodics, and antidepressants.
- Bladder instillations: Medications are directly instilled into the bladder to reduce inflammation or desensitize nerve endings.
- Neuromodulation therapies: Sacral nerve stimulation and posterior tibial nerve stimulation can modulate nerve signals and reduce pain.
Emerging treatments under investigation include gene therapy, stem cell therapy, and novel drug targets aimed at addressing the underlying mechanisms of BPS/IC. The future of treatment will likely involve a more personalized approach based on understanding individual patient characteristics and tailoring therapies accordingly. Continued research is crucial to unraveling the complexities of these conditions and developing more effective treatments. What Is the Best Pain Relief for UTI Flare-Ups? can also provide some relief in certain cases.