Chronic prostatitis pain can be debilitating, significantly impacting quality of life for those who experience it. Often, conventional treatments don’t fully address the persistent discomfort, leading individuals to seek a deeper understanding of what might be happening within their nervous system. This article explores the concept of central sensitization as it relates to chronic prostatitis pain, aiming to provide clarity on this complex phenomenon and how it may contribute to ongoing symptoms even after initial inflammation has subsided.
The experience of chronic pain is rarely straightforward. It’s not simply a matter of damaged tissue sending signals to the brain; the brain itself plays a crucial role in processing and modulating these signals. Understanding this interplay between physical sensations and neurological processes is key to comprehending conditions like chronic prostatitis pain, where the persistence of symptoms often extends beyond what initial tissue damage would predict.
What is Central Sensitization?
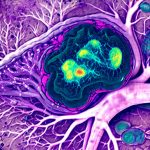
Central sensitization refers to an altered state of nervous system function that develops after prolonged or intense stimulation. Essentially, it’s a process where the central nervous system—the brain and spinal cord—becomes hypersensitive. This heightened sensitivity can lead to amplified pain responses, even from normally non-painful stimuli, and can contribute to widespread pain experiences. It’s not “imaginary” pain; it is a genuine neurophysiological change.
This isn’t an immediate reaction but develops over time with persistent nociceptive input (signals indicating potential or actual tissue damage). The nervous system, in attempting to protect itself, recalibrates its thresholds for pain perception, making it more reactive and less efficient at modulating discomfort.
Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) & Central Sensitization
Chronic prostatitis is often categorized into different types, with CP/CPPS being particularly complex. This syndrome frequently involves pelvic pain, urinary symptoms, and sexual dysfunction without evidence of bacterial infection or inflammation in many cases. The persistent nature of the pain and its associated symptoms strongly suggests a role for central sensitization in a significant proportion of individuals experiencing CP/CPPS.
Mechanisms Linking Prostatitis & Central Sensitization
The initial inflammatory processes associated with prostatitis, even if mild or subclinical, can trigger the cascade leading to central sensitization. Repeated flares, nerve irritation within the prostate and surrounding structures, and pelvic floor dysfunction all contribute to ongoing nociceptive input. Over time, this sustained stimulation alters neuronal circuits in the spinal cord and brain, lowering pain thresholds and expanding areas of sensitivity. This isn’t limited to the pelvis; sensitized systems can exhibit referred pain or hyperalgesia (increased sensitivity to touch) in distant locations.
Furthermore, psychological factors such as stress, anxiety, and depression are closely intertwined with central sensitization. These emotional states can amplify pain perception and hinder the nervous system’s natural ability to dampen down signals. The interplay between physical sensations, psychological state, and neurological changes is crucial in understanding the chronic nature of CP/CPPS symptoms.
Identifying Potential Central Sensitization Indicators
Recognizing indicators suggestive of central sensitization isn’t always straightforward, but certain signs can point towards its involvement. These include allodynia (pain from normally non-painful stimuli like light touch), hyperalgesia (exaggerated pain response to mildly painful stimuli), widespread pain beyond the prostate region, and a discrepancy between objective findings (like imaging results) and reported pain intensity. Fatigue, sleep disturbances, cognitive difficulties (“fibro fog”), and emotional distress are also commonly associated with central sensitization.
It’s important to note that these indicators do not definitively diagnose central sensitization; they suggest its potential contribution to the overall pain experience. A thorough evaluation by a healthcare professional is essential for accurate assessment.
Therapeutic Approaches Targeting Central Sensitization
Addressing central sensitization requires a multimodal approach that goes beyond simply targeting peripheral inflammation or tissue damage. Treatments often focus on modulating nervous system function, reducing pain signaling, and improving coping mechanisms. Physical therapy focusing on pelvic floor muscle relaxation and coordination can reduce nerve irritation and restore proper biomechanics. Cognitive Behavioral Therapy (CBT) helps individuals manage pain catastrophizing, improve coping strategies, and address psychological factors contributing to the pain experience.
Other potential therapies include graded motor imagery, which aims to retrain the brain’s perception of movement and body image; mindfulness-based stress reduction techniques; and potentially certain medications that can modulate neuronal excitability. The key is to understand that this isn’t about “curing” central sensitization but rather learning to manage it and restore a more balanced nervous system function, allowing for improved functionality and quality of life.
The complexity of chronic pain conditions like CP/CPPS necessitates a holistic understanding that acknowledges the interplay between physical, neurological, and psychological factors. Central sensitization provides a valuable framework for appreciating how persistent pain can develop and persist even in the absence of ongoing tissue damage. By recognizing the potential role of central sensitization, individuals and healthcare professionals can collaborate on more effective and targeted treatment strategies aimed at restoring function and improving quality of life. It’s crucial to remember that chronic pain management is often a journey requiring patience, self-compassion, and a willingness to explore different approaches tailored to individual needs.