Urinary tract infections (UTIs) are incredibly common, affecting millions annually, and often dismissed as simply inconvenient. However, for some individuals, recurrent UTIs become a frustrating and debilitating part of life, prompting investigation beyond the typical bacterial causes. While most UTIs stem from E. coli entering the urinary tract, increasingly, healthcare professionals are recognizing that underlying immune dysfunction can play a significant role—and autoimmune disorders may be a key piece of this puzzle. Understanding the complex interplay between immunity, inflammation, and UTI susceptibility is crucial for effective management and long-term relief.
The traditional understanding of UTIs focuses on bacterial virulence and host defenses centered around a healthy urinary tract microbiome and robust immune response. But what happens when that immune response isn’t functioning optimally? Autoimmune disorders, by their very nature, disrupt the delicate balance of the immune system, leading to chronic inflammation and impaired function. This can create a vulnerability not just to infections in general, but specifically impact the ability to effectively clear bacteria from the urinary tract, or even contribute to symptoms that mimic UTI without bacterial presence—a condition sometimes called “unexplained recurrent UTIs.” This article delves into how autoimmune conditions might increase susceptibility to UTIs and explores potential connections between them.
The Autoimmune System & Urinary Tract Vulnerability
Autoimmune disorders arise when the immune system mistakenly attacks the body’s own tissues, perceiving them as foreign invaders. Conditions like rheumatoid arthritis, lupus, Sjögren’s syndrome, multiple sclerosis, and inflammatory bowel disease all fall under this umbrella. This misdirected attack leads to chronic inflammation, which can compromise various bodily functions, including those crucial for preventing UTIs. The urinary tract, while possessing inherent defense mechanisms, relies on a functional immune system to effectively combat invading bacteria.
- A compromised immune response may struggle to quickly identify and eliminate pathogens in the urinary tract.
- Chronic inflammation associated with autoimmune diseases can damage the bladder lining, making it more susceptible to bacterial adhesion and infection.
- Some autoimmune medications – particularly immunosuppressants used to manage these conditions – further weaken the immune system, exacerbating UTI risk.
It’s important to note that this isn’t a simple cause-and-effect relationship. It’s often a confluence of factors; an individual with an autoimmune disorder may experience increased UTI frequency due to a weakened immune response combined with other predisposing factors like anatomical variations or hormonal changes. The type of autoimmune disease, its severity, and the specific treatments being used all contribute to the level of risk. Therefore, understanding the nuances of each patient’s condition is vital for appropriate management.
Specific Autoimmune Conditions & UTI Links
Certain autoimmune conditions appear to have stronger links to recurrent UTIs than others. Sjögren’s syndrome, an autoimmune disease that primarily affects moisture-producing glands, stands out as a significant risk factor. This is because the dryness caused by Sjögren’s directly impacts the urinary tract, reducing natural flushing and creating a more favorable environment for bacterial growth. Lupus, another systemic autoimmune disease, can affect the kidneys (lupus nephritis), further complicating UTI diagnosis and treatment. Inflammatory bowel diseases like Crohn’s disease and ulcerative colitis may also contribute to UTIs due to altered gut microbiome composition and potential immune dysregulation affecting distant sites like the urinary tract.
Furthermore, the medications used to manage these conditions often have immunosuppressive effects. For example:
1. Corticosteroids suppress the immune system broadly.
2. Disease-modifying antirheumatic drugs (DMARDs) alter immune function.
3. Biologic therapies target specific components of the immune system.
These medications, while essential for managing autoimmune disease symptoms, can inadvertently increase susceptibility to infections, including UTIs. It’s a delicate balancing act – weighing the benefits of immunosuppression against the risk of infection requires careful monitoring and collaboration between patients and their healthcare providers. Recognizing this connection allows for proactive strategies aimed at minimizing UTI risk in individuals with autoimmune disorders.
The Role of Chronic Inflammation
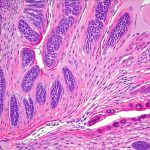
Chronic inflammation is a hallmark feature of all autoimmune diseases, and its impact on urinary tract health shouldn’t be underestimated. Persistent inflammation can damage the bladder epithelium—the protective lining of the bladder—making it more permeable and prone to bacterial colonization. This damage isn’t always visible or immediately symptomatic; it can gradually erode the natural defenses of the urinary tract over time, leading to recurrent infections.
- Inflammation alters the microbiome within the urinary tract, potentially disrupting the balance between beneficial and harmful bacteria.
- Inflammatory cytokines (signaling molecules) released by the immune system can interfere with the normal function of bladder cells, reducing their ability to eliminate pathogens.
- Chronic inflammation can also contribute to pelvic floor dysfunction, which may impair complete bladder emptying, increasing the risk of bacterial overgrowth.
Addressing chronic inflammation is therefore a key component of managing UTI susceptibility in individuals with autoimmune disorders. This might involve strategies beyond traditional antibiotic treatment, such as dietary modifications, stress management techniques, and therapies aimed at modulating the immune system.
Impact of Immunosuppressive Medications
As previously mentioned, many medications used to manage autoimmune diseases suppress the immune system, increasing vulnerability to infections. These medications aren’t always avoidable—they are often essential for controlling disease activity and preventing long-term complications. However, understanding their impact on immune function is critical for proactive UTI prevention.
It’s important that patients taking immunosuppressants:
1. Discuss with their physician the potential risks and benefits of these medications.
2. Practice diligent hygiene—especially after using the restroom.
3. Stay well-hydrated to promote urinary flushing.
Furthermore, healthcare providers should consider adjusting medication dosages or exploring alternative therapies when possible, particularly in patients experiencing frequent UTIs. Prophylactic antibiotics (low-dose antibiotics taken regularly to prevent infections) may be considered in some cases, but their long-term use carries its own risks and should be carefully evaluated.
Exploring “Unexplained” Recurrent UTIs
A growing number of individuals experience recurrent UTI symptoms without evidence of bacterial infection on standard urine cultures – often termed “unexplained recurrent UTIs.” In these cases, autoimmune dysfunction is increasingly suspected as a contributing factor. The chronic inflammation associated with autoimmune diseases can cause bladder irritation and pain that mimics UTI symptoms, even in the absence of bacteria.
- This phenomenon highlights the importance of comprehensive evaluation beyond traditional urine cultures.
- Diagnostic tests to assess immune function and identify underlying autoimmune conditions may be warranted in patients with unexplained recurrent UTIs.
- Management strategies for these types of UTIs often differ from those used for bacterial infections, focusing on reducing inflammation, restoring bladder health, and addressing any underlying autoimmune triggers.
It’s crucial to remember that this information is intended for general knowledge and informational purposes only, and does not constitute medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of any medical condition.