Understanding Bladder Cancer & Its Potential Impact on Energy Levels
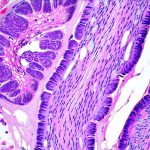
Bladder cancer, while not always discussed openly, affects thousands of individuals annually. It’s a disease that originates in the cells lining the bladder – the organ responsible for storing urine. Symptoms often present initially as blood in the urine (hematuria), but the disease’s impact can extend far beyond this easily identifiable sign. Many people living with bladder cancer experience a range of debilitating side effects, and one increasingly recognized issue is profound fatigue. This isn’t simply feeling tired after a long day; it’s a pervasive exhaustion that interferes significantly with daily life, impacting physical function, emotional wellbeing, and overall quality of life.
The relationship between bladder cancer and fatigue is complex and multifaceted. It’s not always directly linked to the cancer itself, but often stems from the disease’s treatment – surgery, chemotherapy, radiation therapy, or a combination thereof. However, even before treatment begins, some individuals experience fatigue related to the underlying disease process itself. This article aims to explore this connection in detail, examining the various contributing factors and offering insights for managing this challenging symptom. Understanding why bladder cancer can cause fatigue is the first step toward effectively addressing it and reclaiming a better quality of life during and after treatment.
The Multifaceted Roots of Fatigue in Bladder Cancer
Fatigue in bladder cancer patients isn’t a single phenomenon; rather, it’s a constellation of factors working together. One significant contributor is the physical toll of treatment modalities. Surgery, particularly radical cystectomy (removal of the entire bladder), requires substantial recovery time and can lead to chronic pain and functional limitations. Chemotherapy and radiation therapy, while targeting cancer cells, also impact healthy cells, leading to side effects that drain energy reserves. These treatments often disrupt sleep patterns, further exacerbating fatigue. Beyond these direct treatment effects, the emotional burden of a cancer diagnosis – anxiety, depression, fear about recurrence – can contribute significantly to feelings of exhaustion.
Another critical aspect is the potential for anemia resulting from bladder cancer or its treatment. Blood in the urine, even if not visibly apparent, can lead to iron deficiency over time, and chemotherapy frequently suppresses bone marrow function, reducing red blood cell production. Anemia reduces oxygen delivery to tissues, leading to weakness and fatigue. Furthermore, changes in metabolism associated with cancer itself – including increased energy expenditure by tumor cells – can deplete the body’s resources. The body is constantly working harder just to maintain basic functions, leaving less energy available for daily activities.
Finally, it’s essential to recognize that inflammation plays a substantial role. Cancer and its treatment trigger an inflammatory response in the body, which, while intended to fight the disease, can also contribute to fatigue. Chronic inflammation consumes significant energy and disrupts normal physiological processes. This creates a vicious cycle where inflammation leads to fatigue, and fatigue weakens the immune system, potentially worsening inflammation. Managing these intertwined factors is key to mitigating fatigue and improving patient wellbeing.
Understanding Treatment-Related Fatigue
Treatment for bladder cancer often involves aggressive interventions that have inherent side effects, many of which directly contribute to fatigue. Chemotherapy, for instance, doesn’t just target cancerous cells – it impacts rapidly dividing healthy cells as well, including those in the bone marrow responsible for blood cell production. This can lead to chemotherapy-induced anemia, a common cause of debilitating fatigue. Radiation therapy, similarly, can damage surrounding tissues and organs, causing pain, inflammation, and exhaustion.
- Surgical interventions such as radical cystectomy are physically demanding, requiring significant recovery time.
- The reconstruction process following bladder removal (e.g., creating a neobladder or ileal conduit) further adds to the physical strain on the body.
- Postoperative pain management can also contribute to fatigue, both directly through its draining effects and indirectly through medication side effects.
Furthermore, the psychological stress associated with treatment – fear of recurrence, anxiety about side effects, disruption of daily routines – can amplify feelings of fatigue. It’s important for patients undergoing bladder cancer treatment to proactively communicate their levels of fatigue to their healthcare team. Early identification allows for adjustments to treatment plans (if possible) and implementation of supportive care strategies like pain management, nutritional counseling, and psychological support.
The Role of Anemia & Nutritional Deficiencies
Anemia is a frequent companion to bladder cancer, arising from several sources. As mentioned previously, blood in the urine – even microscopic amounts – can result in chronic iron loss over time. This leads to iron-deficiency anemia, characterized by insufficient red blood cells to carry oxygen effectively throughout the body. Chemotherapy and radiation therapy further compound this issue by directly suppressing bone marrow function, hindering red blood cell production. The symptoms of anemia – fatigue, weakness, shortness of breath, dizziness – often mimic those of cancer itself, making it challenging to differentiate between the two.
Beyond iron deficiency, other nutritional deficiencies can also exacerbate fatigue. Cancer and its treatment frequently lead to loss of appetite, nausea, and vomiting, making it difficult for patients to maintain adequate nutrition. Deficiencies in vitamins (e.g., vitamin D, B vitamins) and minerals (e.g., magnesium, zinc) can further compromise energy levels. Addressing these nutritional deficiencies is vital – a registered dietitian specializing in oncology can provide personalized guidance on dietary modifications and potential supplementation strategies.
- Regular blood tests to monitor hemoglobin levels and identify any nutrient deficiencies are essential.
- Dietary adjustments may include increasing iron-rich foods (lean meats, beans, leafy greens) and ensuring adequate protein intake.
- Supplementation should only be done under the guidance of a healthcare professional.
Managing Fatigue: A Holistic Approach
There’s no single cure for fatigue in bladder cancer patients, but there are numerous strategies that can help manage it effectively. A holistic approach, addressing both physical and emotional factors, is often most successful. This starts with open communication with your healthcare team – reporting your fatigue levels honestly allows them to assess the situation and tailor a management plan to your specific needs.
- Physical activity, even gentle exercise like walking or yoga, can paradoxically increase energy levels over time. It’s crucial to start slowly and gradually increase intensity as tolerated.
- Prioritize sleep. Establish a regular sleep schedule, create a relaxing bedtime routine, and address any underlying sleep disturbances.
- Nutrition plays a key role. Focus on a balanced diet rich in protein, vitamins, and minerals. Consider consulting with a registered dietitian specializing in oncology for personalized recommendations.
Beyond these lifestyle modifications, psychological support can be invaluable. – Cognitive behavioral therapy (CBT) can help patients develop coping mechanisms for managing fatigue and anxiety. – Support groups provide a safe space to connect with others facing similar challenges. Finally, explore available resources like occupational or physical therapy to address functional limitations and improve overall wellbeing. Remember that managing fatigue is an ongoing process, requiring patience, self-compassion, and collaboration with your healthcare team.