Bladder inflammation, clinically known as cystitis, is often perceived as a straightforward infection typically caused by bacteria like E. coli. While this remains a common cause, it’s increasingly recognized that the origins of cystitis are far more complex and can stem from deeper immune system imbalances. Many individuals experience recurrent or chronic bladder issues that don’t respond to traditional antibiotic treatments, hinting at underlying mechanisms beyond simple bacterial infection. These persistent cases frequently point toward a disconnect between the immune system and the urinary tract, where the body’s defense mechanisms either malfunction, overreact, or become desensitized leading to inflammation.
The intricate relationship between the immune system and bladder health is now a burgeoning area of research. A healthy immune system normally recognizes and neutralizes pathogens effectively, preventing infection from taking hold. However, when the immune system isn’t functioning optimally – due to factors like autoimmune conditions, chronic stress, or nutritional deficiencies – it can create an environment where inflammation persists even in the absence of active bacterial presence. Understanding this interplay is crucial for developing effective long-term strategies for managing bladder health and moving beyond solely treating symptoms to addressing root causes.
The Immune System’s Role in Bladder Health
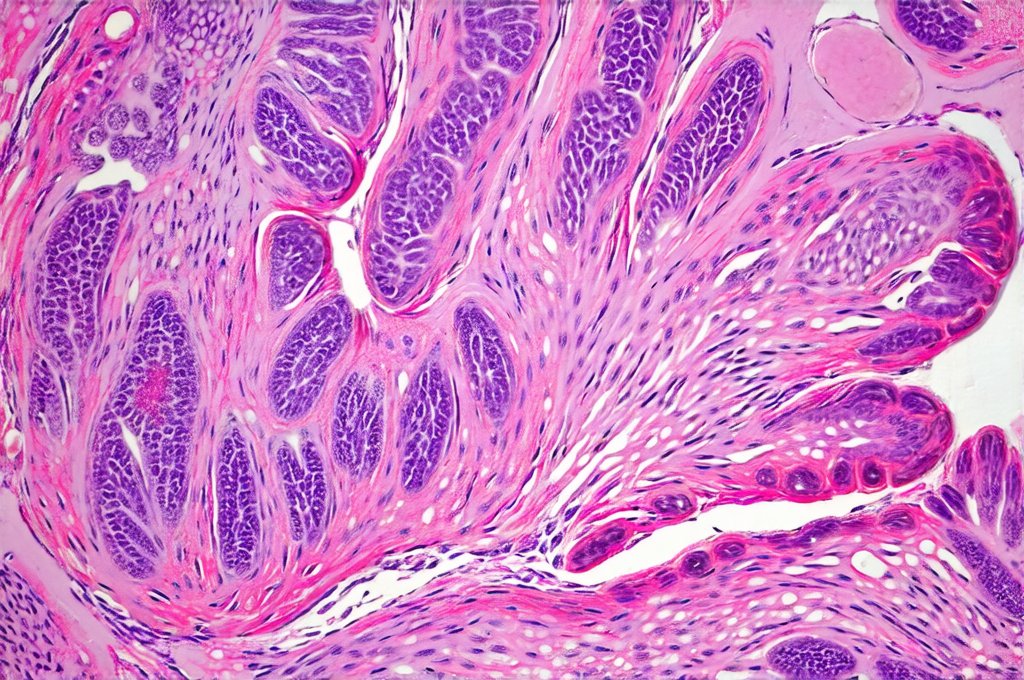
The urinary tract isn’t sterile, as once believed; it harbors a microbiome, albeit different from the gut. A healthy immune system maintains a delicate balance within this ecosystem, preventing harmful bacteria from overgrowing and causing infection. Key components of the immune response in the bladder include innate immunity – the first line of defense involving physical barriers like the urothelium (bladder lining) and cells like macrophages which engulf pathogens – and adaptive immunity, where T and B cells learn to recognize specific threats and mount targeted responses. When this system is compromised, the bladder becomes vulnerable to chronic inflammation.
Autoimmune diseases are particularly relevant here. Conditions like Lupus, Sjögren’s syndrome, or rheumatoid arthritis can cause systemic immune dysregulation, increasing susceptibility to bladder inflammation as the immune system mistakenly attacks healthy tissues. Even without a diagnosed autoimmune disease, chronic low-grade inflammation throughout the body – often fueled by factors like poor diet, stress, and environmental toxins – can weaken the immune response in the urinary tract, making it harder for the bladder to defend itself. This creates a vicious cycle where persistent inflammation further suppresses immune function.
Furthermore, the gut microbiome profoundly impacts systemic immunity. A disrupted gut microbiome (dysbiosis) can lead to increased intestinal permeability (“leaky gut”), allowing inflammatory molecules to enter the bloodstream and contribute to chronic inflammation throughout the body, including in the urinary tract. Restoring a healthy gut microbiome through diet and probiotics is increasingly recognized as an important adjunct therapy for managing bladder health. Considering the link between gut health and UTIs, exploring can utis be caused by poor gut health can offer valuable insights.
Potential Immune-Related Triggers of Bladder Inflammation
Beyond autoimmune conditions, several other immune system dysfunctions can trigger or exacerbate bladder inflammation. Mast cell activation syndrome (MCAS), where mast cells release excessive amounts of inflammatory mediators, has been linked to chronic pelvic pain and urinary frequency/urgency – symptoms often associated with cystitis. Similarly, imbalances in cytokine production—small signaling molecules that regulate the immune response—can play a significant role. For example, elevated levels of pro-inflammatory cytokines like IL-6 and TNF-alpha can contribute to persistent inflammation even without bacterial infection.
Food sensitivities and allergies are also emerging as potential triggers. When an individual consumes a food they’re sensitive or allergic to, it can trigger an immune response that leads to systemic inflammation, potentially affecting the bladder. Identifying and eliminating these trigger foods through elimination diets can sometimes significantly improve symptoms. Finally, chronic stress profoundly impacts immunity. Prolonged stress releases cortisol, which suppresses immune function and increases susceptibility to infection and inflammation. Managing stress through techniques like mindfulness, yoga, or meditation is therefore an important part of a holistic approach to bladder health.
Identifying Immune Dysfunction: Diagnostic Approaches
Diagnosing the underlying cause of bladder inflammation beyond bacterial infection requires a more comprehensive assessment. Traditional urine cultures may not reveal anything in cases of non-bacterial cystitis, necessitating further investigation. – One key test is assessing inflammatory markers in the urine and blood, such as cytokines and C-reactive protein (CRP), to identify elevated levels indicating immune activation.
-
Complete Blood Count (CBC) with differential can help evaluate overall immune cell function and detect signs of autoimmune activity. – Stool testing for microbiome analysis can reveal imbalances in gut bacteria that might be contributing to systemic inflammation. – Allergy and sensitivity testing, including IgG food sensitivity tests or elimination diets guided by a healthcare professional, can identify potential triggers.
-
Specialized tests like mast cell activation syndrome (MCAS) panels are available but often require specialist interpretation. It’s important to note these tests aren’t always conclusive, and diagnosis often relies on clinical evaluation alongside test results. A functional medicine or integrative medicine practitioner experienced in autoimmune and immune disorders can be particularly helpful in navigating these diagnostic complexities. Understanding how hormones might affect UTIs is also crucial; can utis be triggered by hormonal pills in women provides further insight into this connection.
The Role of Urothelial Dysfunction & Immune Cell Interactions
The urothelium isn’t just a passive barrier; it actively participates in the immune response. It secretes antimicrobial peptides and expresses receptors that recognize pathogens, initiating an immune cascade when threatened. However, chronic inflammation can damage the urothelium, compromising its protective functions and leading to increased permeability—allowing more irritants to reach underlying tissues. This creates further inflammation, establishing a feedback loop.
Immune cells within the bladder wall, like macrophages and T cells, play a critical role in this process. In healthy individuals, these cells effectively clear pathogens and resolve inflammation. However, in cases of immune dysfunction, their activity can become dysregulated. Macrophages might release excessive inflammatory molecules, while T cells may attack urothelial cells, exacerbating the damage. The interplay between these cells and the urothelium is complex, and understanding it is key to developing targeted therapies.
Addressing Immune Dysfunction: Potential Therapies
Managing bladder inflammation triggered by immune dysfunction requires a multifaceted approach focused on restoring immune balance and reducing inflammation. – Dietary interventions: An anti-inflammatory diet rich in fruits, vegetables, omega-3 fatty acids, and probiotics can support gut health and reduce systemic inflammation. Eliminating food sensitivities identified through testing or elimination diets is also crucial.
-
Stress management techniques: Mindfulness, yoga, meditation, and deep breathing exercises can help regulate cortisol levels and improve immune function. – Supplementation: Certain supplements may support immune function and reduce inflammation, including Vitamin D, curcumin (from turmeric), quercetin, and omega-3 fatty acids. However, it’s essential to consult with a healthcare professional before starting any new supplements.
-
Immunomodulatory therapies: In some cases, specific immunomodulatory treatments – under the guidance of an experienced practitioner – may be necessary. These could include low-dose naltrexone (LDN), which can help regulate immune function, or intravenous vitamin C therapy to support immune cell activity. – Addressing gut health: Probiotic supplementation and dietary changes aimed at restoring a healthy gut microbiome can significantly impact systemic immunity and bladder health. Can UTI pain be triggered by bowel movements highlights the potential connection between digestive health and urinary symptoms, further emphasizing the importance of a holistic approach. It’s important to remember that there is no one-size-fits-all approach, and treatment plans should be individualized based on the specific underlying cause of immune dysfunction.