Bladder dysfunction impacts millions worldwide, ranging from mild inconvenience to severely debilitating conditions affecting quality of life. Traditional approaches often involve medication or, in more severe cases, surgical intervention. However, an increasing number of individuals are discovering the potential benefits of bladder retraining – a behavioral therapy aimed at restoring normal bladder function without resorting to invasive treatments. This approach recognizes that many bladder issues stem from learned behaviors and habits, and seeks to “re-educate” both the bladder and the brain to work in harmony.
The core principle behind bladder retraining is based on gradually increasing the time between voiding, challenging the bladder’s capacity and ultimately restoring a more functional volume. It’s not about holding urine until discomfort – it’s about strategically lengthening intervals, coupled with techniques to manage urgency and reduce anxiety around bladder control. This method can be particularly effective for conditions like urge incontinence (a sudden, strong need to urinate) and overactive bladder (OAB), where the bladder contracts involuntarily. Success hinges on consistent effort, patience, and a clear understanding of the retraining process.
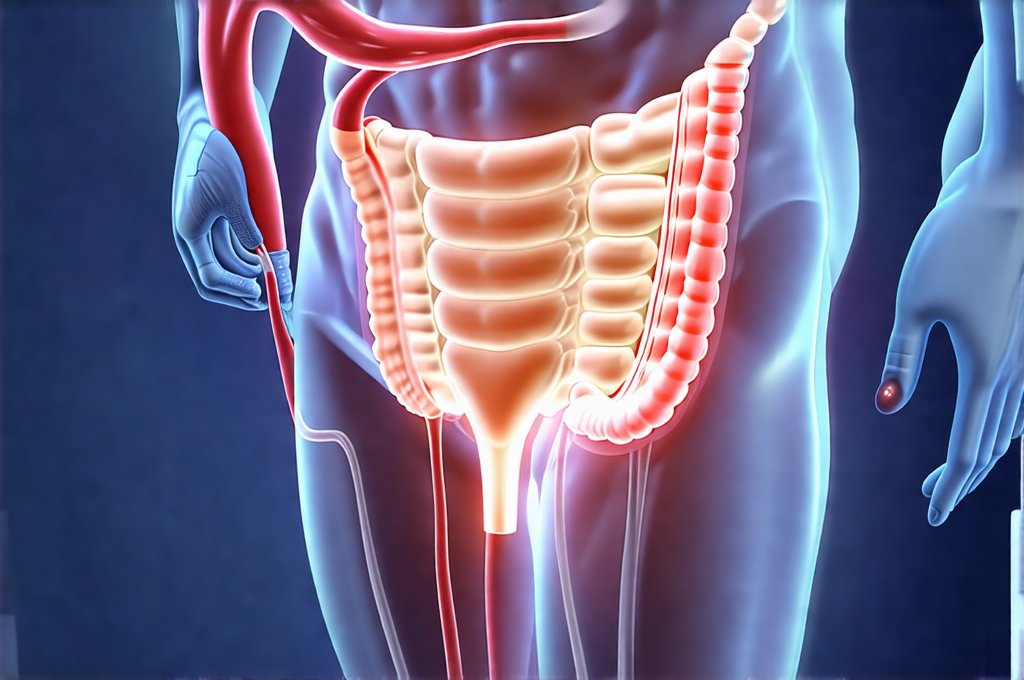
Understanding Bladder Function & Dysfunction
The urinary system is a complex network responsible for storing and eliminating waste. The bladder, a muscular organ, expands as it fills with urine produced by the kidneys. Nerves signal to the brain when the bladder reaches a certain level of fullness, creating the urge to urinate. Normally, we can consciously control this urge until a convenient time and place. However, in cases of dysfunction, this control is compromised. Several factors can contribute to these issues, including nerve damage, weakened pelvic floor muscles, hormonal changes, or even behavioral patterns that have inadvertently trained the bladder to empty at lower volumes.
- Urge Incontinence: Characterized by a sudden, intense urge to urinate followed by involuntary leakage. Often linked to overactive bladder.
- Stress Incontinence: Leakage occurs during physical exertion like coughing, sneezing, or exercise—caused by weakened pelvic floor muscles.
- Overactive Bladder (OAB): A frequent and urgent need to urinate, even when the bladder isn’t full, potentially leading to urge incontinence.
- Functional Incontinence: Difficulty reaching a toilet in time due to physical limitations or cognitive impairments.
Bladder retraining specifically addresses issues related to urgency and frequency often associated with OAB and urge incontinence. It doesn’t directly address stress incontinence, which requires different interventions like pelvic exercises. The goal is to increase the bladder’s functional capacity – the amount of urine it can comfortably hold – and to regain control over the urge to void.
How Bladder Retraining Works: A Step-by-Step Approach
Bladder retraining isn’t a quick fix; it requires consistent effort and adherence to a structured program. It typically involves several stages, beginning with bladder diaries to establish baseline habits. These diaries track fluid intake, urination times, urgency levels (on a scale of 1-5), and any leakage episodes. This data provides valuable insight into individual patterns and helps tailor the retraining plan. Following diary monitoring, the core retraining process begins:
- Timed Voiding: Initially, patients are instructed to void at fixed intervals, regardless of urge – for example, every hour or two. This establishes a regular pattern.
- Gradual Interval Increase: As tolerance improves, the time between scheduled voids is gradually increased by 15-30 minutes each week. The aim is to slowly stretch the bladder’s capacity and reduce frequency.
- Urge Suppression Techniques: When urgency arises before the scheduled voiding time, techniques like pelvic floor muscle contractions (Kegels), deep breathing exercises, or distraction are employed to suppress the urge until the designated time.
- Positive Reinforcement: Celebrating successes – even small ones – is crucial for maintaining motivation and building confidence.
Throughout the process, it’s essential to avoid excessive fluid intake, limit caffeine and alcohol (which can irritate the bladder), and address any underlying factors contributing to dysfunction. It’s also vital to remember that setbacks are normal; consistency and a positive attitude are key to long-term success.
Addressing Urgency & Reducing Anxiety
Urgency is often the most challenging aspect of bladder retraining, as it triggers anxiety and can lead to involuntary leakage. Learning effective urge suppression techniques is therefore paramount. One powerful technique involves performing quick pelvic floor muscle contractions (Kegels). The idea isn’t to hold the contraction indefinitely but rather to use a series of short, rapid squeezes to temporarily calm the bladder muscles and reduce the sensation of urgency.
Another valuable tool is diaphragmatic breathing. Slow, deep breaths from the diaphragm can activate the parasympathetic nervous system – often referred to as the “rest and digest” system – which helps to counteract the fight-or-flight response associated with urgency. Practicing these techniques regularly, even when not experiencing an urgent sensation, builds muscle memory and makes them more readily available during moments of need. Furthermore, distraction can be surprisingly effective. Focusing on something else—counting backwards, reciting a poem, or mentally visualizing a calming scene—can temporarily divert attention from the urge and allow it to subside.
The Role of Pelvic Floor Muscle Exercises (Kegels)
While bladder retraining focuses primarily on behavioral modification, integrating pelvic floor muscle exercises significantly enhances its effectiveness. These muscles support the bladder, urethra, and other pelvic organs, providing crucial stability and control. Weakened pelvic floor muscles contribute to both stress and urge incontinence, so strengthening them is essential for restoring function.
- Proper Technique: Kegels involve contracting the muscles you would use to stop the flow of urine midstream. It’s vital to avoid engaging abdominal or gluteal muscles during the exercise.
- Frequency & Duration: Aim for sets of 10-15 contractions, several times throughout the day. Gradually increase the hold time and repetitions as strength improves.
- Consistency is Key: Like any exercise program, consistent practice is vital to see results.
It’s important to note that incorrectly performed Kegels can be ineffective or even counterproductive. Seeking guidance from a physical therapist specializing in pelvic floor health ensures proper technique and personalized recommendations. Combining Kegels with bladder retraining creates a synergistic effect, addressing both the muscular and behavioral components of bladder dysfunction.
Long-Term Maintenance & Potential Limitations
Once significant improvements are achieved through bladder retraining, long-term maintenance is crucial to prevent relapse. This involves continuing timed voids (though potentially at wider intervals), practicing urge suppression techniques regularly, and maintaining a healthy lifestyle that supports bladder health. Regular follow-up with a healthcare professional can provide ongoing support and address any emerging issues.
However, it’s important to acknowledge the limitations of bladder retraining. It may not be effective for all individuals or conditions. For example, those with severe nerve damage affecting bladder control might require alternative treatments. Additionally, adherence to the program requires significant commitment and discipline, which can be challenging for some. Bladder retraining is most effective when integrated as part of a comprehensive treatment plan developed in consultation with a healthcare professional. While it offers a promising non-invasive approach to restoring bladder function, it’s not a one-size-fits-all solution but rather a personalized strategy requiring patience, consistency, and ongoing support. It’s also important to understand that mild bladder irritation can sometimes develop into more serious conditions if left untreated.