Cystitis, commonly understood as a bladder infection, is often swiftly attributed to bacterial causes and treated accordingly with antibiotics. While this approach effectively addresses many cases, an increasing body of evidence suggests that cystitis isn’t always so straightforward. For a significant number of individuals – particularly women experiencing recurrent infections – the root cause may lie deeper than simple bacterial overgrowth. This leads us to explore the possibility that certain types of cystitis could be manifestations of underlying autoimmune dysregulation, where the immune system mistakenly attacks healthy tissues within the urinary tract, or even triggers inflammatory responses mimicking infection.
The conventional understanding of cystitis often overlooks the complexity of the immune system’s role in maintaining bladder health. Autoimmune conditions are notoriously difficult to diagnose, often presenting with vague and fluctuating symptoms that can easily be mistaken for other ailments. The chronic inflammation associated with autoimmune diseases can significantly impact the urinary tract’s delicate balance, predisposing individuals to persistent discomfort and recurrent ‘infections.’ This is not necessarily an infection in the traditional sense, but rather a consequence of immune system misfiring – a critical distinction often missed in routine medical assessments. It’s important to remember that this exploration isn’t about self-diagnosis; it’s about understanding the broader possibilities when conventional treatments fail or provide only temporary relief. Can cystitis be a side effect of menstruation? may offer further insights into recurring issues.
The Interplay Between Immunity and Bladder Health
The bladder, despite its role as a storage reservoir for urine, is not immune to the influence of the body’s larger immunological landscape. A healthy bladder maintains a delicate balance between protective immunity and tolerance – recognizing and responding appropriately to threats while avoiding unnecessary inflammation. However, in autoimmune conditions, this balance can be disrupted, leading to chronic inflammation even without the presence of an invading pathogen. This is where the lines between recurrent cystitis and autoimmune disease begin to blur. Individuals with systemic autoimmune diseases like Lupus or Sjögren’s syndrome are more prone to urinary tract issues, but even without a formal diagnosis of such conditions, localized autoimmunity within the bladder itself can occur.
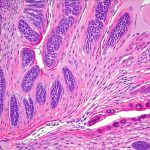
The urothelium, the specialized lining of the bladder, plays a vital role in immune regulation. It isn’t just a passive barrier; it actively participates in immune responses and communicates with immune cells. In autoimmune scenarios, this communication can become aberrant, triggering an inappropriate inflammatory cascade. This chronic inflammation damages the urothelium, making it more susceptible to irritation and further exacerbating symptoms that mimic infection. Furthermore, certain genetic predispositions can increase susceptibility to both autoimmune conditions and recurrent cystitis, suggesting a shared underlying vulnerability. Is chronic cystitis a form of autoimmune disease? explores this connection in more detail.
The diagnosis of autoimmune-related cystitis is challenging because traditional urine cultures may come back negative, even when symptoms are severe. This often leads to repeated rounds of antibiotics, which offer temporary relief but ultimately fail to address the root cause – the misdirected immune response. The focus then shifts from treating an infection to investigating potential immunological factors contributing to the chronic inflammation.
Potential Autoimmune Conditions Linked to Cystitis-Like Symptoms
Several autoimmune conditions are known to manifest with urinary tract symptoms that closely resemble cystitis. These aren’t necessarily direct consequences of bladder infection, but rather expressions of systemic immune dysregulation impacting the urinary system. Lupus, for example, can cause glomerulonephritis (inflammation of kidney filters) and interstitial cystitis-like symptoms, including pelvic pain and urinary frequency. Sjögren’s syndrome, which primarily affects moisture-producing glands, can lead to bladder dysfunction and increased susceptibility to urinary tract discomfort. However, the most direct link often appears in cases resembling Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS).
IC/BPS is a chronic condition characterized by pelvic pain, urinary urgency, and frequency without evidence of infection. While its exact cause remains unknown, growing research suggests that autoimmune factors play a significant role in at least a subset of IC/BPS cases. Studies have identified elevated levels of autoantibodies – antibodies that mistakenly target the body’s own tissues – in some patients with IC/BPS. These autoantibodies can attack urothelial cells, leading to chronic inflammation and pain. Furthermore, immune cell infiltration into bladder tissue is commonly observed in individuals with IC/BPS, indicating an ongoing autoimmune response. Identifying these immunological markers is crucial for differentiating IC/BPS from simple bacterial cystitis and guiding more targeted treatment approaches.
It’s important to note that diagnosing autoimmune-related cystitis requires a comprehensive evaluation by a healthcare professional, including detailed medical history, physical examination, urine analysis (including testing for autoantibodies), and potentially bladder biopsies. This process can be complex and time-consuming, but it’s essential for accurately identifying the underlying cause of symptoms and developing an appropriate treatment plan.
Investigating Autoimmunity in Chronic Cystitis Cases
When recurrent cystitis persists despite repeated antibiotic courses, a deeper investigation into potential autoimmune factors is warranted. – One crucial step is to review the patient’s medical history for any signs of other autoimmune conditions or family history of such diseases. – Blood tests can be ordered to assess levels of autoantibodies associated with various autoimmune disorders, as well as markers of inflammation like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
However, standard autoimmune antibody panels may not always be sufficient in identifying localized autoimmunity within the bladder. More specialized testing might be necessary, such as examining urine for specific autoantibodies targeting urothelial cells or conducting a bladder biopsy to assess immune cell infiltration and tissue damage. Immunohistochemistry on bladder biopsies can help identify specific immune cells present in the bladder wall, providing valuable clues about the underlying autoimmune process. Can frequent urination be a sign of kidney stones? highlights other potential causes for urinary frequency and discomfort.
It’s also important to consider other factors that can mimic autoimmune cystitis, such as pelvic floor dysfunction, nerve entrapment, or food sensitivities. A thorough differential diagnosis is crucial for avoiding misdiagnosis and ensuring appropriate treatment. The role of gut health shouldn’t be ignored either; imbalances in the gut microbiome have been linked to both autoimmune conditions and urinary tract symptoms.
Treatment Approaches for Autoimmune-Related Cystitis
Treating cystitis stemming from an autoimmune basis differs significantly from conventional antibiotic therapy. – The primary goal is to modulate the immune system, reduce inflammation, and restore bladder health. This often involves a multi-faceted approach tailored to the individual patient’s specific needs and underlying condition. Immunosuppressant medications, such as low-dose naltrexone or other immunomodulatory drugs, might be considered in severe cases under the strict guidance of a rheumatologist or immunologist.
However, less aggressive interventions can also be effective for many patients. These include dietary modifications to reduce inflammation (e.g., eliminating processed foods, sugar, and gluten), stress management techniques, and pelvic floor physical therapy. Supplements with anti-inflammatory properties, such as curcumin or omega-3 fatty acids, may also provide some relief. Addressing gut health through probiotic supplementation and dietary changes can further support immune regulation.
It’s crucial to remember that treatment for autoimmune-related cystitis is often a long-term process requiring ongoing management and monitoring. Regular follow-up with healthcare professionals is essential to adjust the treatment plan as needed and ensure optimal outcomes.
The Future of Cystitis Research and Diagnosis
The understanding of cystitis is evolving, recognizing its complexity beyond simple bacterial infections. Increased research into the immunological aspects of bladder health will undoubtedly lead to more accurate diagnostic tools and targeted therapies. – Advances in biomarker discovery are crucial for identifying individuals with autoimmune-related cystitis early on, before significant tissue damage occurs.
Developing non-invasive methods for assessing bladder immune function would also be a significant step forward. Furthermore, personalized medicine approaches, tailoring treatment to the individual patient’s genetic and immunological profile, hold great promise for improving outcomes. Ultimately, recognizing that cystitis can be a symptom of underlying autoimmune dysregulation is essential for providing comprehensive and effective care to those suffering from this debilitating condition. The future lies in moving beyond one-size-fits-all treatments and embracing a more holistic and nuanced understanding of bladder health. Can recurrent UTIs Be a Sign of Bladder Cancer? explores other serious conditions that can mimic UTI or cystitis symptoms, emphasizing the importance of comprehensive diagnostics.