Cystitis, commonly understood as a urinary tract infection (UTI), is often associated with bacterial causes. However, the reality is far more nuanced. While Escherichia coli remains the most frequent culprit, cystitis can arise from various factors, including irritation and inflammation triggered by sensitivities or allergies. This leads many to question if seemingly unrelated exposures – like those encountered during intimate activity – could contribute to developing this uncomfortable condition. The increasing awareness of latex allergies, coupled with widespread condom use for contraception and protection against sexually transmitted infections (STIs), naturally brings up the question: can cystitis develop from an allergic reaction to condoms?
The connection isn’t always straightforward, as it rarely presents as a typical infection. Instead, individuals experiencing sensitivity or allergy to condom materials might experience symptoms mimicking cystitis – frequent urination, urgency, burning sensations, and discomfort in the pelvic region – but stemming from irritation rather than bacterial invasion. This can be incredibly confusing, both for those experiencing these symptoms and for healthcare professionals attempting diagnosis. It’s crucial to differentiate between a true UTI requiring antibiotic treatment and an inflammatory response caused by allergic or irritant contact dermatitis, which requires a different approach to management.
Understanding the Link Between Condoms & Bladder Irritation
The primary concern when linking condoms to cystitis-like symptoms revolves around the materials used in their construction. The vast majority of condoms are made from latex, a natural rubber derived from the Hevea brasiliensis tree. While effective as a barrier against STIs and pregnancy, latex is a known allergen for many individuals – estimates suggest between 1% and 6% of the population experiences a latex allergy. Even those without a full-blown allergy can experience sensitivity to latex, resulting in contact dermatitis. Beyond latex, condoms may also contain other potential irritants like spermicides (nonoxynol-9), fragrances, or preservatives used during manufacturing. These additives increase the likelihood of triggering an adverse reaction in susceptible individuals.
It’s important to note that a true allergic reaction involves the immune system and can range from mild localized reactions (like itching and rash) to severe systemic responses like anaphylaxis – though this is rare with condom use. More commonly, the symptoms related to condoms are due to irritant contact dermatitis, which isn’t an immune response but rather direct irritation of sensitive tissues by the materials themselves. This irritation can affect the urethra, vagina, or surrounding areas and mimic UTI symptoms when inflammation extends to the bladder region. The close proximity of the urethra to these areas makes it easy for external irritants to cause discomfort that feels remarkably like cystitis.
Furthermore, friction during intercourse, particularly if insufficient lubrication is used, can exacerbate irritation from condom materials. This mechanical stress, combined with chemical sensitivity, creates a perfect storm for inflammation and discomfort. The use of scented lubricants or douches may further aggravate the situation, disrupting the natural vaginal flora and increasing susceptibility to irritation. Therefore, identifying the root cause – allergy, sensitivity, friction, or a combination thereof – is essential for appropriate management.
Alternative Condom Materials & Reducing Irritation
Recognizing that latex isn’t suitable for everyone, manufacturers have introduced alternative condom materials. Polyisoprene, polyurethane, and polyurethanes are all non-latex options available today. Polyisoprene closely mimics the feel of latex but doesn’t contain the allergy-causing proteins found in natural rubber. Polyurethane is thinner than both latex and polyisoprene, offering increased sensitivity but can be more prone to tearing if not used with adequate lubrication. Polyurethanes are often considered a good compromise between comfort and durability.
Switching to an alternative condom material is often the first step in managing symptoms related to condom sensitivities. However, even with non-latex condoms, it’s crucial to choose options free from fragrances, spermicides (nonoxynol-9), and other potentially irritating additives. Reading the product label carefully and opting for hypoallergenic varieties can make a significant difference. It’s also important to remember that even alternative materials can cause irritation in some individuals; personal tolerance varies greatly.
Beyond material choice, several strategies can help minimize irritation: – Use ample water-based lubricant during intercourse. Avoid oil-based lubricants as they can degrade latex and polyurethane condoms. – Ensure proper condom application to avoid friction and pressure on sensitive tissues. – Practice good hygiene before and after sexual activity. – Consider avoiding douching or using harsh soaps in the genital area, which disrupt the natural balance of flora. – If symptoms persist despite these measures, consult a healthcare professional for further evaluation and personalized recommendations. Understanding how to distinguish cystitis from vaginitis can also help pinpoint the source of discomfort.
Identifying Allergy vs. Sensitivity
Differentiating between an allergy and sensitivity can be tricky as both present with similar symptoms. However, understanding their underlying mechanisms helps guide appropriate action. An allergy involves the immune system recognizing a substance (like latex protein) as harmful and mounting an immune response – often including histamine release which causes itching, swelling, hives, or even anaphylaxis in severe cases. Allergic reactions typically occur consistently upon exposure to the allergen.
A sensitivity, on the other hand, doesn’t involve the immune system. It’s a direct reaction of tissues to irritants like chemicals or friction. Symptoms are usually localized and less severe than allergic reactions. Sensitivity may develop over time with repeated exposure and can vary in intensity depending on factors like hydration levels and skin barrier function.
To help determine if you have an allergy, consider undergoing allergy testing. A healthcare provider can perform a skin prick test or blood test to assess your immune response to latex. However, negative results don’t necessarily rule out sensitivity; they simply indicate the absence of an allergic reaction. Paying attention to when symptoms occur and what factors exacerbate them is key for self-assessment. For example, if symptoms consistently appear after using latex condoms but not with non-latex options, it strongly suggests a latex allergy or sensitivity. It’s also important to know how to recognize allergic reactions generally.
When To Seek Medical Attention
While many cases of condom-related irritation can be managed with simple adjustments like switching materials and increasing lubrication, it’s crucial to seek medical attention when symptoms are severe or persistent. If you experience any of the following, consult a healthcare professional: – Severe itching, swelling, hives, or difficulty breathing (signs of an allergic reaction). – Painful urination that doesn’t improve after several days. – Fever, chills, back pain, or nausea – these could indicate a true UTI requiring antibiotic treatment. – Bleeding or unusual discharge from the vagina or urethra.
A healthcare provider can accurately diagnose the cause of your symptoms and recommend appropriate treatment. This may involve prescribing antihistamines for allergic reactions, topical corticosteroids to reduce inflammation, or antibiotics if a bacterial infection is present. It’s important not to self-treat with antibiotics, as this contributes to antibiotic resistance and won’t address irritation caused by allergies or sensitivities. If you are concerned about recurring UTIs, learning how to distinguish UTI from interstitial cystitis can be helpful.
Preventing Future Flare-Ups
Once you’ve identified the cause of your symptoms, proactive steps can prevent future flare-ups. This includes consistently using hypoallergenic condoms made from suitable materials. Maintaining a healthy lifestyle – staying hydrated, eating a balanced diet, and managing stress levels – strengthens the immune system and skin barrier function, reducing susceptibility to irritation.
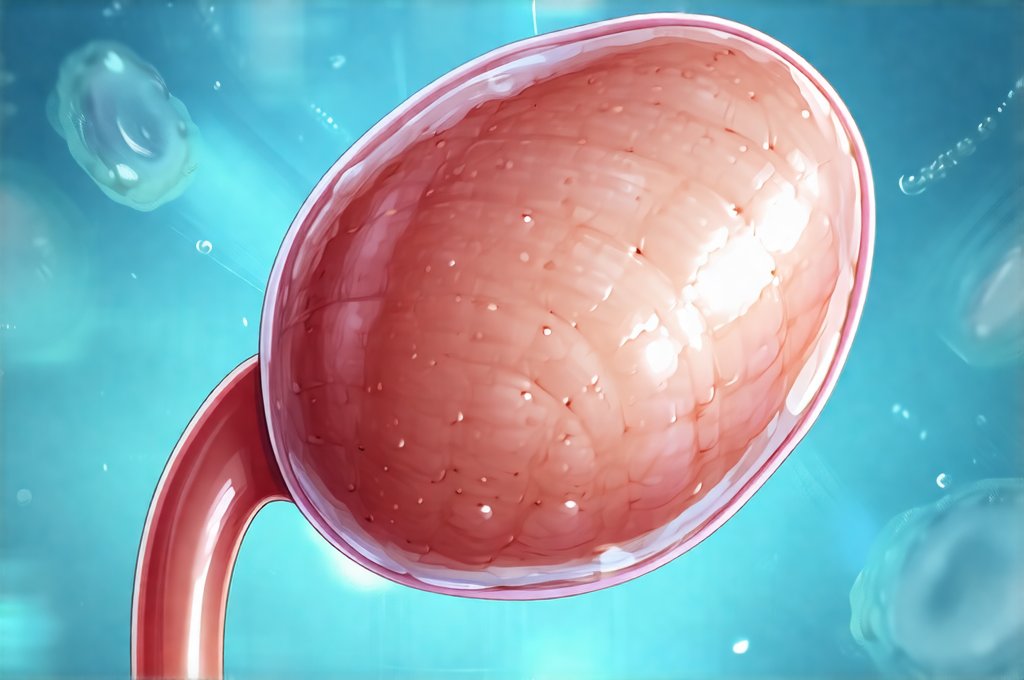
Furthermore, open communication with sexual partners about sensitivities and preferences is essential. This ensures mutual comfort and allows for collaborative decision-making regarding protection methods. Remember that prioritizing your health and well-being is paramount. Don’t hesitate to explore alternative options and seek professional guidance when needed. Ultimately, understanding the connection between condoms, allergies, sensitivities, and bladder irritation empowers individuals to make informed choices and enjoy a healthy sexual life without discomfort. It can also be helpful to understand what to expect from an ultrasound if diagnostic imaging is needed.