Chronic bladder problems, encompassing conditions like interstitial cystitis (IC) or painful bladder syndrome, can be incredibly debilitating, impacting quality of life significantly. Often, the search for answers leads patients down a path of symptom management without addressing underlying causes. While traditionally viewed as localized issues within the urinary tract, emerging research increasingly points to a more systemic connection – specifically, the gut microbiome and associated inflammation. The intricate bidirectional communication between the gut and bladder, often referred to as the “gut-bladder axis,” is now being recognized as a potential key player in the development and perpetuation of these chronic conditions.
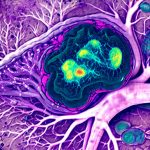
The prevailing understanding of bladder dysfunction has historically focused on localized factors like nerve sensitivity, muscle abnormalities, or autoimmune responses within the bladder itself. However, this limited perspective fails to account for the significant influence of the gut microbiome – the trillions of bacteria residing in our digestive tract – on systemic inflammation and immune function. A disrupted gut microbiome (dysbiosis) can lead to increased intestinal permeability (“leaky gut”), allowing bacterial products and toxins to enter the bloodstream, triggering chronic low-grade inflammation that affects distant organs, including the bladder. This paradigm shift opens up new avenues for investigation and potential therapeutic interventions beyond traditional symptom management.
The Gut-Bladder Axis: A Two-Way Street
The connection between the gut and bladder isn’t a one-way street; it’s a complex interplay of neurological, immunological, and hormonal signaling pathways. Neurotransmitters like serotonin and substance P, which play crucial roles in pain perception and inflammation, are significantly influenced by the gut microbiome. In fact, a substantial portion of the body’s serotonin is produced in the gut. Gut dysbiosis can disrupt neurotransmitter balance, potentially leading to heightened sensitivity to bladder signals and increased pain experience. Furthermore, the immune system, heavily influenced by the gut microbiome, plays a critical role in both protecting against infection and contributing to chronic inflammation. An imbalanced gut microbiome can trigger an overactive or misdirected immune response, exacerbating bladder symptoms.
The vagus nerve serves as a direct communication pathway between the gut and brain, influencing bladder function indirectly through its impact on nervous system regulation. Hormonal imbalances, also linked to gut health, can contribute to bladder dysfunction. For example, estrogen levels, influenced by the microbiome’s ability to modulate hormone metabolism, are known to affect bladder sensitivity and urgency. This interconnectedness explains why individuals with irritable bowel syndrome (IBS), a common condition associated with gut dysbiosis, often experience co-occurring bladder symptoms. Understanding this complex axis is vital for developing holistic treatment strategies that address the root causes of chronic bladder problems rather than simply masking the symptoms.
The role of specific microbial metabolites also contributes to this axis. Short-chain fatty acids (SCFAs), produced by beneficial gut bacteria during fiber fermentation, possess anti-inflammatory properties and can modulate immune function, potentially protecting the bladder from inflammation. Conversely, harmful bacterial metabolites can exacerbate inflammation and contribute to bladder dysfunction. Therefore, modulating the microbiome through dietary changes or targeted therapies could offer a novel approach to managing chronic bladder conditions. Recognizing that are painful periods linked to these issues can help patients understand connections between seemingly unrelated symptoms.
Gut Inflammation & Bladder Dysfunction: Mechanisms at Play
Chronic low-grade inflammation originating in the gut can directly impact bladder health through several mechanisms. Increased intestinal permeability, as previously mentioned, allows for systemic dissemination of bacterial components like lipopolysaccharide (LPS), a potent inflammatory trigger. LPS activates immune cells throughout the body, including those within the bladder wall, leading to chronic inflammation and heightened sensitivity. This inflammatory cascade can damage urothelial cells – the lining of the bladder – contributing to increased permeability and pain perception.
Another key mechanism involves mast cell activation. Mast cells, immune cells residing in tissues throughout the body (including the bladder), are highly sensitive to gut-derived inflammatory signals. Activation of mast cells releases histamine and other inflammatory mediators, further amplifying inflammation within the bladder and exacerbating symptoms like urgency, frequency, and pain. Furthermore, alterations in the microbiome can influence the production of cytokines – signaling molecules that regulate immune responses. An imbalance in cytokine profiles, driven by gut dysbiosis, can contribute to chronic inflammation and impaired bladder function.
Research is also exploring the role of autoimmunity in chronic bladder problems. A “leaky gut” allows for increased exposure to antigens (foreign substances), potentially triggering an autoimmune response where the immune system mistakenly attacks healthy bladder tissues. This autoimmune component, fueled by gut-derived inflammation, could contribute to the persistent and often debilitating symptoms associated with conditions like interstitial cystitis. It’s important to note that can low immunity may also play a role here.
Identifying Gut Inflammation: Diagnostic Approaches
Pinpointing gut inflammation as a contributing factor requires a multifaceted diagnostic approach. Standard stool testing can identify dysbiosis – imbalances in the microbiome composition – but doesn’t always reveal the extent of inflammation. More advanced tests, such as fecal calprotectin and zonulin levels, can provide insights into intestinal inflammation and permeability, respectively. Elevated calprotectin indicates active inflammation within the gut, while high zonulin suggests increased intestinal permeability (“leaky gut”).
Beyond stool analysis, blood tests can assess markers of systemic inflammation, such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). However, these markers are non-specific and don’t necessarily pinpoint the gut as the source of inflammation. Comprehensive digestive health assessments, which combine stool testing with dietary analysis and symptom assessment, offer a more holistic evaluation of gut function and inflammation. It’s crucial to remember that diagnostic tests should be interpreted by a healthcare professional who understands the complexities of the gut-bladder axis.
Dietary Interventions for Gut Health & Bladder Support
Diet plays a pivotal role in modulating gut health and reducing inflammation. A diet rich in fiber from fruits, vegetables, and whole grains promotes the growth of beneficial gut bacteria, leading to increased SCFA production and improved immune function. Conversely, a diet high in processed foods, sugar, and unhealthy fats can contribute to dysbiosis and inflammation. Eliminating common food sensitivities – such as gluten, dairy, or soy – may also help reduce gut inflammation for some individuals.
Specific dietary strategies tailored to bladder support include reducing intake of bladder irritants like caffeine, alcohol, spicy foods, and acidic beverages (citrus fruits, tomatoes). Increasing water intake is crucial for diluting urine and minimizing bladder irritation. Probiotic-rich foods – such as yogurt, kefir, sauerkraut, and kimchi – can help replenish beneficial gut bacteria, but it’s important to choose strains that have been shown to support urinary tract health. Prebiotics, found in foods like onions, garlic, and asparagus, provide nourishment for beneficial gut bacteria.
Restoring Gut Health: Therapeutic Strategies
Beyond dietary changes, several therapeutic strategies can help restore gut health and reduce inflammation. Probiotic supplementation can be a valuable tool, but it’s crucial to select strains based on individual needs and consult with a healthcare professional. Different probiotic strains have different effects, and what works for one person may not work for another. Other interventions include glutamine supplementation, which helps repair the gut lining, and herbal remedies like curcumin (from turmeric) and ginger, known for their anti-inflammatory properties.
Fecal Microbiota Transplantation (FMT) – transferring stool from a healthy donor to a recipient – is an emerging therapy showing promise in restoring gut microbiome diversity and reducing inflammation. However, FMT is typically reserved for severe cases of recurrent Clostridium difficile infection and is not yet widely used for chronic bladder problems. Finally, stress management techniques like yoga, meditation, and mindfulness can help reduce cortisol levels, which can negatively impact gut health and immune function. A holistic approach that addresses both the gut microbiome and lifestyle factors is essential for long-term success in managing chronic bladder conditions. Additionally, understanding can microclots contribute to these issues can give a more complete picture of potential underlying causes.