Chronic prostatitis, a condition affecting millions of men worldwide, presents a complex diagnostic and therapeutic challenge. Characterized by persistent pelvic pain, urinary dysfunction, and often psychological distress, its etiology remains incompletely understood. Traditional explanations have centered around infection, inflammation, nerve damage, and autoimmune processes, but increasingly researchers are exploring novel mechanisms potentially contributing to the development and perpetuation of this frustrating condition. One emerging area of investigation focuses on microclots – tiny blood clots that can form within capillaries – and their potential role in chronic prostatitis symptoms. This article will delve into the current understanding of microclots, how they might relate to prostate health, and what research is being conducted to explore these connections.
The complexity surrounding chronic prostatitis stems from its varied presentation and often elusive causes. It’s not always linked to bacterial infection (in fact, most cases aren’t), making diagnosis and targeted treatment difficult. This has spurred investigation into alternative pathways contributing to the condition’s persistence – including examining subtle disruptions in blood flow and microvascular function that may not be readily apparent through conventional testing. Understanding these mechanisms is crucial for developing more effective strategies for managing this challenging health issue.
The Emerging Role of Microclots
Microclots are small, often undetectable formations within the capillaries—the smallest blood vessels in the body. They aren’t the large, easily identifiable clots associated with strokes or deep vein thrombosis; instead, they represent a subtle disruption to normal blood flow at the microvascular level. Their formation can be triggered by various factors, including inflammation, endothelial dysfunction (damage to the lining of blood vessels), and altered blood viscosity. While initially studied in contexts like stroke and cardiovascular disease, growing research suggests their potential involvement in conditions ranging from chronic fatigue syndrome to long COVID.
The precise mechanisms behind microclot formation are still being elucidated, but it’s thought they involve interactions between platelets, fibrinogen (a protein crucial for clotting), and red blood cells. These microclots can physically obstruct capillaries, reducing oxygen delivery to tissues, or release substances that contribute to inflammation and further vascular damage – creating a potentially self-perpetuating cycle.
Potential Connections to Chronic Prostatitis
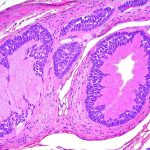
The link between microclots and chronic prostatitis isn’t yet fully established, but several lines of reasoning suggest a possible connection. The prostate gland has a rich blood supply, making it vulnerable to disruptions in microvascular function. Furthermore, chronic inflammation – a hallmark of many prostatitis cases – can promote microclot formation. If the prostate doesn’t receive adequate oxygen and nutrients due to capillary obstruction by microclots, it could contribute to tissue damage, pain, and impaired function—mirroring some of the symptoms experienced in chronic prostatitis.
Microvascular Dysfunction and Prostate Health
The health of the prostate gland is intimately tied to its blood supply. Effective circulation ensures proper nutrient delivery and waste removal, supporting optimal cellular function. Microclots can compromise this delicate balance by reducing capillary density and impairing blood flow. This diminished perfusion could lead to localized hypoxia (oxygen deprivation) within the prostate tissue, potentially exacerbating inflammation and pain sensations. Studies in other chronic pain conditions have shown a correlation between microvascular dysfunction and increased symptom severity; similar mechanisms might be at play in chronic prostatitis.
Inflammation as a Catalyst
Chronic inflammation is central to many instances of chronic prostatitis. Inflammatory processes can damage the endothelial lining of blood vessels, making them more prone to microclot formation. Furthermore, inflammatory mediators released during an immune response can actually activate platelets and promote fibrin deposition—the building blocks of clots. This creates a feedback loop where inflammation drives microclotting, which in turn worsens tissue damage and further fuels inflammation. The prostate’s unique anatomical location and susceptibility to inflammation (due to factors like urinary tract infections or pelvic floor dysfunction) could make it particularly vulnerable to this cycle.
Research & Future Directions
Current research into the role of microclots in chronic prostatitis is still in its early stages, but several studies are beginning to explore this connection. Some investigations are focused on identifying biomarkers indicative of microclot presence and activity in patients with chronic prostatitis. Others are examining whether interventions aimed at improving microvascular function – such as lifestyle modifications promoting endothelial health (exercise, diet) or therapies targeting platelet activation—can alleviate symptoms. Advanced imaging techniques capable of visualizing microcirculation may also play a role in confirming the presence of microclots within the prostate gland and assessing their impact on tissue perfusion.
More research is necessary to definitively determine whether microclots are a causative factor in chronic prostatitis, a consequence of the condition, or simply coexist with it. However, this emerging area holds promise for unlocking new therapeutic avenues and improving our understanding of this complex and debilitating condition. It’s important to note that self-diagnosis and treatment should be avoided; any concerns about chronic prostatitis should be discussed with a qualified healthcare professional.