Prostatitis, inflammation of the prostate gland, is a common condition affecting men of all ages, though more frequently those over 50. While often attributed to bacterial infection, a significant portion of cases fall under the umbrella of chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), where no clear infectious cause can be identified. This leaves many patients and clinicians grappling with understanding the underlying mechanisms driving persistent symptoms like pain, urinary dysfunction, and sexual discomfort. Increasingly, researchers are exploring connections between CP/CPPS and broader systemic conditions characterized by chronic immune activation and dysregulation, leading to questions about whether prostatitis could represent a localized manifestation of more widespread inflammatory processes.
The complexity of CP/CPPS necessitates looking beyond traditional infectious etiologies. The elusive nature of the condition suggests that factors beyond bacterial presence play a crucial role in its development and persistence. This exploration has led to investigations into potential autoimmune components, nerve sensitization, pelvic floor dysfunction, and, importantly, systemic inflammatory responses. Understanding these connections is vital for developing more effective diagnostic and therapeutic strategies for men experiencing chronic prostate issues.
Chronic Inflammatory Response Syndrome (CIRS): An Overview
Chronic Inflammatory Response Syndrome, or CIRS, describes a constellation of symptoms arising from prolonged exposure to various environmental triggers – often mold and biotoxins – leading to immune dysregulation and systemic inflammation. It’s not simply an allergic reaction but rather a complex interplay between the body’s attempts to deal with ongoing stimuli and its resulting inflammatory cascade. Individuals experiencing CIRS often present with fatigue, cognitive dysfunction (“brain fog”), musculoskeletal pain, headaches, and various gastrointestinal issues, mirroring symptoms seen in many chronic conditions.
CIRS is characterized by an overactive immune response that struggles to return to baseline even after the initial trigger is removed. This ongoing inflammation can impact multiple organ systems, leading to a wide range of seemingly disparate symptoms. Diagnostic criteria for CIRS are still evolving and remain somewhat controversial within mainstream medicine, but it’s gaining recognition as a potential underlying factor in many chronic illnesses.
The Potential Link Between Prostatitis and Systemic Inflammation
The increasing research into CP/CPPS has begun to highlight parallels between the condition and systemic inflammatory states like CIRS. Both conditions demonstrate evidence of immune activation, elevated inflammatory markers (though often subtle and inconsistent), and a tendency toward neurological symptoms alongside physical discomfort. Importantly, many men experiencing chronic prostatitis also report significant fatigue, cognitive issues, and generalized pain – symptoms frequently associated with CIRS. The possibility that underlying systemic inflammation could exacerbate or even initiate CP/CPPS is a growing area of investigation.
Immune Dysregulation in Both Conditions
Both CP/CPPS and CIRS involve disruptions to the immune system’s normal functioning. In CIRS, persistent exposure to environmental triggers leads to an overstimulated immune response with impaired regulatory mechanisms. Similarly, in CP/CPPS, even without a clear bacterial infection, there’s evidence of immune cell infiltration into the prostate gland and elevated levels of pro-inflammatory cytokines – signaling molecules that amplify inflammation. This suggests that the body’s normal ability to regulate inflammatory responses is compromised in both conditions. Studies have shown increased levels of T helper 1 cells (associated with cellular immunity) and altered cytokine profiles in men with CP/CPPS, mirroring some of the immune imbalances seen in CIRS patients.
The Role of Mast Cells
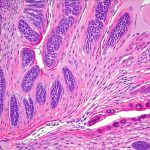
Mast cells are key players in both inflammation and immune responses. They release histamine and other inflammatory mediators, contributing to symptoms like pain, swelling, and increased sensitivity. In CIRS, mast cell activation is considered a central feature of the illness, driving many of the observed symptoms. Interestingly, evidence suggests that mast cell activation may also play a significant role in CP/CPPS. Studies have found elevated mast cell numbers in prostate tissue samples from men with chronic prostatitis, indicating their involvement in the inflammatory process. This overlap raises questions about whether similar mechanisms – perhaps driven by environmental triggers or other systemic factors – are contributing to both conditions.
Neurological Manifestations and Sensitization
Chronic inflammation often leads to neurological symptoms due to its impact on the nervous system. In CIRS, “brain fog,” headaches, and cognitive dysfunction are common complaints. Similarly, CP/CPPS frequently involves pelvic pain that can become chronic and debilitating, contributing to nerve sensitization – a process where nerves become hypersensitive to stimuli. This heightened sensitivity can lead to ongoing pain even in the absence of continued inflammation. The connection between systemic inflammation, mast cell activation, and neurological symptoms is increasingly recognized as a key factor in both CIRS and CP/CPPS, suggesting a shared underlying pathway. It’s plausible that chronic inflammatory processes could contribute to central sensitization—a state where the brain amplifies pain signals—in both conditions.
Ultimately, while research continues to unfold, recognizing the potential connection between prostatitis (specifically CP/CPPS) and Chronic Inflammatory Response Syndrome offers a broader perspective on this complex condition. It emphasizes the importance of considering systemic factors beyond localized prostate inflammation when evaluating men with chronic pelvic pain and urinary symptoms. Further investigation into immune function, mast cell activation, and neurological implications may pave the way for more comprehensive and effective treatment approaches that address the underlying causes rather than solely focusing on symptom management. A holistic approach to patient care, considering environmental exposures, lifestyle factors, and overall health status, is likely crucial in managing both CIRS and CP/CPPS effectively.