Chronic cystitis – inflammation of the bladder – isn’t simply a urinary tract infection that keeps coming back. It’s often a complex condition with multiple contributing factors, and managing it effectively requires a holistic approach extending far beyond antibiotics. Many individuals living with chronic cystitis find their daily routines significantly disrupted by pain, urgency, frequency, and fatigue. This can lead to social isolation, anxiety, and reduced quality of life. Understanding how seemingly small adjustments to your daily routine can impact symptom management is crucial for regaining control and improving wellbeing. The goal isn’t necessarily a “cure” – as chronic cystitis often requires ongoing management – but rather finding strategies to minimize flare-ups and live a fuller, more comfortable life despite the condition.
This article explores practical ways to adjust your daily routine to better navigate chronic cystitis. It focuses on adaptable lifestyle changes that support bladder health and overall wellbeing, recognizing that everyone experiences this condition differently. These aren’t one-size-fits-all solutions; they are starting points for experimentation and personalization. We’ll delve into aspects of diet, hydration, activity levels, stress management, and sleep hygiene, all with the aim of empowering you to take an active role in managing your symptoms and improving your day-to-day life. Remember that consulting with a healthcare professional is essential for personalized guidance and treatment plans. Considering routine adjustments can be very beneficial.
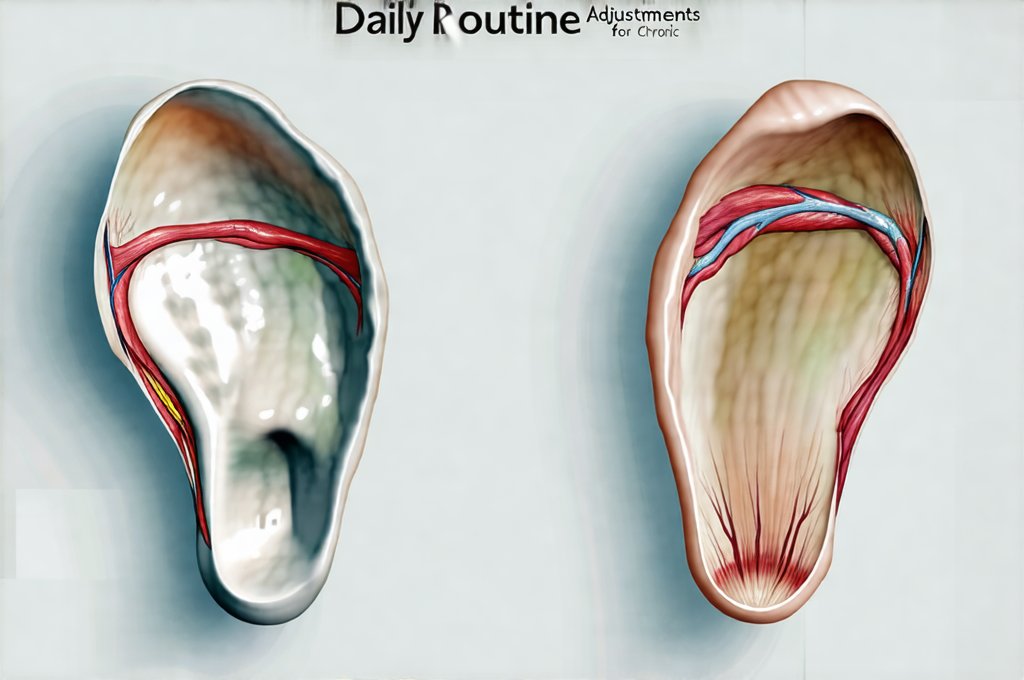
Dietary Adaptations for Bladder Health
Diet plays a surprisingly large role in cystitis symptom management. Certain foods and drinks can irritate the bladder lining, exacerbating urgency, frequency, and pain. Identifying your personal triggers is key – what bothers one person may not bother another. A common starting point is to eliminate or significantly reduce consumption of known bladder irritants, then slowly reintroduce them one at a time to observe any reactions. – Caffeine (coffee, tea, soda) – Alcohol – Citrus fruits and juices – Spicy foods – Artificial sweeteners – Tomato-based products – including sauces and ketchup – Carbonated beverages are also often problematic.
Beyond avoiding triggers, incorporating bladder-soothing foods can be beneficial. Foods rich in antioxidants may help reduce inflammation. Many people find relief from consuming alkaline-forming foods, as an acidic environment can irritate the bladder. This isn’t about completely changing your diet overnight but making mindful choices that support bladder health. Consider increasing intake of: – Water (of course!) – we’ll discuss hydration more later – Blueberries – Pears – Bananas – Oatmeal – Almonds. A food diary can be incredibly helpful in tracking what you eat and correlating it with symptom fluctuations, allowing you to identify your personal dietary triggers effectively. Learning how to build a balanced daily routine can also help improve diet.
Hydration Strategies & Bowel Regularity
Adequate hydration is essential, but the “eight glasses a day” rule isn’t always appropriate for chronic cystitis. Drinking excessive amounts of fluid can actually increase frequency and urgency. The goal is to find the sweet spot – enough fluid to stay hydrated without overstimulating the bladder. Sipping water consistently throughout the day, rather than drinking large volumes at once, is generally better tolerated. Pay attention to your body’s signals and adjust intake accordingly. Monitoring urine color can be a helpful guide; pale yellow indicates adequate hydration. However, it’s important to note that some medications or supplements might affect urine colour.
Bowel regularity is often overlooked but profoundly impacts bladder health. Constipation can put pressure on the bladder, worsening symptoms. A high-fiber diet, regular exercise, and sufficient fluid intake all contribute to healthy bowel movements. If constipation is a persistent issue, discuss it with your healthcare provider – they may recommend gentle laxatives or stool softeners. Conversely, diarrhea can also irritate the bladder, so managing that aspect of digestive health is equally important. Probiotics might be beneficial for both constipation and diarrhea, promoting a balanced gut microbiome.
Managing Pain & Flare-Ups
Chronic cystitis often involves chronic pain, which significantly impacts daily functioning. Developing a proactive pain management strategy is vital. This may involve a combination of approaches: – Heat therapy (warm baths, heating pads) can soothe pelvic muscles and reduce discomfort. – Gentle exercise, like walking or yoga, can help release tension and improve circulation. – Pelvic floor physiotherapy can strengthen and relax the pelvic floor muscles, which play a role in bladder control. – Mindfulness techniques, such as meditation or deep breathing exercises, can help manage pain perception and stress levels.
Flare-ups are inevitable with chronic cystitis, but having a plan in place can minimize their impact. When a flare-up begins, prioritize rest, stay hydrated (but avoid overdoing it), and avoid bladder irritants. Consider reducing activity levels temporarily and practicing self-compassion. Keeping a symptom diary during flare-ups can help identify potential triggers and inform future management strategies. Don’t hesitate to contact your healthcare provider if symptoms are severe or don’t improve with self-care measures. Finding adaptive daily routines is important for managing pain.
Prioritizing Sleep & Reducing Stress
Sleep deprivation exacerbates cystitis symptoms, creating a vicious cycle of pain, fatigue, and disrupted sleep. Establishing a regular sleep schedule, creating a relaxing bedtime routine, and optimizing your sleep environment are crucial. Avoid caffeine and alcohol before bed, create a dark, quiet, and cool bedroom, and consider using relaxation techniques like meditation or deep breathing to calm your mind. If you struggle with insomnia, discuss it with your healthcare provider – they may recommend cognitive behavioral therapy for insomnia (CBT-I) or other sleep aids.
Chronic stress significantly impacts the immune system and can worsen bladder inflammation. Incorporating stress management techniques into your daily routine is essential. This could include: – Regular exercise – Mindfulness meditation – Yoga – Deep breathing exercises – Spending time in nature – Engaging in hobbies you enjoy – Connecting with loved ones. Learning to recognize your personal stressors and developing healthy coping mechanisms are key to managing the emotional toll of chronic cystitis. Remember that seeking support from a therapist or counselor can be incredibly beneficial.
Adapting Activity Levels & Work/Life Balance
Chronic cystitis often necessitates adjustments to activity levels. Pushing yourself too hard when experiencing symptoms can lead to flare-ups, while complete inactivity can contribute to deconditioning and worsen overall health. Finding the right balance is crucial. Listen to your body and pace yourself accordingly. Break down tasks into smaller, more manageable chunks, and don’t be afraid to ask for help when needed. – Prioritize activities that bring you joy and relaxation – even if they are limited in scope. – Avoid strenuous activity during flare-ups. – Consider incorporating gentle exercise, such as walking or swimming, into your routine on days when symptoms are milder.
Work/life balance is often challenging for individuals with chronic conditions. Communicating your needs to your employer and colleagues can help ensure you receive the support you need. This might involve requesting flexible work arrangements, taking breaks throughout the day, or modifying job duties as needed. Setting boundaries and prioritizing self-care are essential for preventing burnout and maintaining wellbeing. Remember that it’s okay to say “no” to commitments that will exacerbate your symptoms or overwhelm you. Daily walk adjustments can help manage activity levels.