Cystitis, an inflammation of the bladder, is a frustrating condition for many, often characterized by painful urination, frequent urges to go, and discomfort in the pelvic region. While commonly associated with bacterial infections, a growing body of evidence suggests that factors beyond infection can significantly impact cystitis flare-ups. Many individuals report experiencing cyclical patterns of symptoms, even after successful treatment for UTIs, leading them to search for underlying triggers. This is where the potential connection between allergies and cystitis comes into play – a complex interplay often overlooked in conventional medical explanations.
The immune system is at the heart of both allergic reactions and inflammatory responses like those seen in cystitis. When an individual encounters an allergen, the body launches a defense mechanism that can sometimes manifest as localized inflammation or even systemic symptoms. Similarly, in non-infectious cystitis, chronic inflammation within the bladder lining appears to be a key driver of symptoms. It’s becoming increasingly recognized that immune dysregulation – where the immune system either overreacts or fails to function optimally – could be a common thread linking allergies and recurring cystitis flare-ups, potentially exacerbating bladder sensitivity and triggering symptom onset. Understanding this potential link is crucial for holistic management and personalized treatment approaches.
The Allergy-Cystitis Connection: A Deeper Dive
The relationship between allergies and cystitis isn’t necessarily about a direct allergic reaction in the bladder itself (though that’s possible, as we’ll discuss later). Instead, it often stems from systemic inflammation triggered by allergies. When someone with allergies is exposed to an allergen – pollen, dust mites, certain foods, pet dander – their immune system releases histamine and other inflammatory chemicals. This isn’t limited to the nose or throat; these chemicals circulate throughout the body, potentially impacting various organs, including the bladder. Chronic, low-grade inflammation from persistent allergies can sensitize the bladder, lowering its threshold for irritation and making it more susceptible to flare-ups even in the absence of a bacterial infection.
This systemic inflammatory burden can affect pelvic floor muscles too. Allergic reactions often contribute to increased muscle tension throughout the body, including the pelvic floor. Tight or dysfunctional pelvic floor muscles can exacerbate bladder symptoms, creating a vicious cycle where inflammation and muscle tension reinforce each other. It’s important to note that this isn’t always a straightforward connection; many people with allergies don’t experience cystitis, and vice versa. However, for individuals who notice symptom correlations, investigating the allergy-cystitis link can be very fruitful.
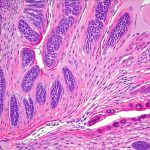
Furthermore, certain allergic responses can impact gut health. Allergic reactions can disrupt the delicate balance of bacteria in the microbiome, leading to leaky gut syndrome – a condition where the intestinal barrier becomes compromised, allowing undigested food particles and toxins to enter the bloodstream. This further fuels systemic inflammation, potentially contributing to cystitis flare-ups. The gut-bladder axis is now recognized as an important factor in bladder health, highlighting how seemingly unrelated systems can be interconnected. What role does biopsy play in diagnosis? can help understand underlying conditions impacting the gut and bladder.
Identifying Allergy Triggers & Their Impact
Pinpointing specific allergy triggers can be challenging, but it’s a vital step in understanding the connection and managing symptoms. Common allergens include: – Food allergies (dairy, gluten, soy, nuts) – Environmental allergens (pollen, dust mites, mold) – Pet dander – Certain chemicals or fragrances. Keeping a detailed symptom diary alongside a record of potential allergen exposures can help identify patterns. For example, someone might notice their cystitis flares up during pollen season or after consuming dairy products.
Allergy testing – skin prick tests or blood tests (IgE antibody tests) – can provide valuable information, but it’s essential to interpret the results cautiously. These tests only identify sensitivities, not necessarily clinically relevant allergies. A positive test doesn’t automatically mean that allergen is causing your cystitis; clinical correlation is crucial. Elimination diets, guided by a healthcare professional, are another method for identifying food sensitivities. This involves removing suspected allergens from the diet and observing whether symptoms improve.
It’s also important to consider non-allergic triggers of inflammation that can mimic allergy symptoms and contribute to cystitis flare-ups. These include stress, hormonal imbalances, certain medications, and underlying autoimmune conditions. A comprehensive evaluation with a healthcare professional is necessary to differentiate between these factors and develop an appropriate management plan. How to tell a bladder infection from cystitis in women can help differentiate these conditions.
Exploring Specific Allergy Types & Cystitis
Food Allergies/Intolerances
Food allergies and intolerances are frequently cited as potential cystitis triggers. While true food allergies (IgE-mediated reactions) are less common, food intolerances – which don’t involve an IgE response but can still cause inflammation – are more prevalent. Common culprits include dairy, gluten, soy, corn, and artificial additives. The inflammatory response triggered by a food intolerance can contribute to systemic inflammation and bladder irritation. – Consider keeping a detailed food diary alongside symptom tracking to identify potential triggers. – An elimination diet, guided by a healthcare professional, may help pinpoint problematic foods. – Focus on an anti-inflammatory diet rich in whole foods, fruits, vegetables, and healthy fats.
Environmental Allergies (Pollen, Dust Mites, Mold)
Seasonal allergies, particularly pollen allergies, can significantly impact bladder health for some individuals. The release of histamine during allergic reactions increases vascular permeability, potentially leading to increased bladder sensitivity and urgency. Similarly, indoor allergens like dust mites and mold can cause chronic inflammation that contributes to cystitis flare-ups. – Implement strategies to minimize allergen exposure: use air purifiers, regularly clean your home, wash bedding frequently, and avoid peak pollen times. – Consider nasal saline rinses to clear allergens from the sinuses. – Explore allergy immunotherapy (allergy shots or sublingual drops) under the guidance of an allergist.
Histamine Intolerance & Bladder Sensitivity
Histamine intolerance is a condition where the body struggles to break down histamine effectively, leading to a buildup and various symptoms, including inflammation and bladder irritation. This can be exacerbated by allergies, as allergic reactions release significant amounts of histamine. Individuals with histamine intolerance may experience increased bladder urgency, frequency, and pain during allergy season or after consuming high-histamine foods (fermented foods, aged cheeses, alcohol). – Identify and avoid high-histamine foods. – Consider supporting histamine breakdown with enzyme supplements (under a healthcare professional’s guidance). – Manage stress, as it can increase histamine release. What role do kegels play in urology for women? may help manage the pelvic floor muscles impacted by histamine intolerance.
It’s important to reiterate that the allergy-cystitis connection is complex and highly individual. What triggers flare-ups for one person may not affect another. A personalized approach, guided by a thorough evaluation and ongoing monitoring, is essential for effective management. Furthermore, this information should not be considered medical advice; always consult with qualified healthcare professionals for diagnosis and treatment of cystitis or allergies. Does vaginal dryness play a role in postmenopausal cystitis? should also be considered if relevant to the patient’s circumstances.