Urinary tract infections (UTIs) are incredibly common, particularly among women, often presenting with frustrating symptoms like frequent urination, burning sensations, and abdominal discomfort. While most people associate UTIs solely with the urinary system, emerging research suggests a surprising interconnectedness between these infections and various skin conditions. This isn’t necessarily about direct infection spreading to the skin; rather, it’s about how the body’s immune response to a UTI, systemic inflammation, and alterations in gut health (often accompanying UTIs or their treatment) can manifest as, or exacerbate, existing dermatological issues. Understanding this link is crucial for holistic healthcare and recognizing that seemingly disparate symptoms might be connected.
The connection isn’t always straightforward; it’s rarely a case of UTI directly causing skin problems in the traditional sense. Instead, it’s more about modulation – UTIs can alter internal processes which then influence the skin’s health and reactivity. This is particularly relevant for individuals already predisposed to conditions like eczema, psoriasis, or acne, where immune system dysregulation plays a significant role. The gut microbiome, heavily impacted by antibiotic use frequently prescribed for UTIs, also has a well-established link with skin health, creating another pathway through which these infections can indirectly affect dermatological wellbeing. We will explore the complex ways in which UTIs and skin conditions interact.
The Immune System & Skin Flare-Ups
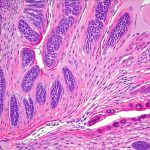
A UTI triggers an immune response as the body attempts to fight off the bacterial infection. This activation of the immune system, while necessary for recovery, can sometimes lead to systemic inflammation – a widespread inflammatory state that doesn’t remain confined to the urinary tract. For individuals with sensitive skin or pre-existing conditions, this systemic inflammation can act as a trigger for flare-ups. – Eczema and atopic dermatitis are prime examples; their symptoms often worsen during periods of increased immune activity. – Psoriasis, another autoimmune-related condition, might experience similar exacerbations. The inflammatory cytokines released during a UTI response (like TNF-alpha and IL-6) can directly contribute to the characteristic skin lesions associated with psoriasis.
The impact isn’t limited to chronic conditions. Even individuals without diagnosed dermatological issues can experience temporary skin reactions. Increased inflammation may lead to general skin sensitivity, redness, or even the development of hives. Antibiotics, frequently used to treat UTIs, further complicate matters. While they address the infection, antibiotics also disrupt the gut microbiome, potentially weakening immune function and contributing to systemic inflammation in the long run. This creates a cyclical effect where treatment for one issue might inadvertently worsen another.
It’s important to remember that not everyone will experience skin flare-ups following a UTI; individual responses vary greatly depending on factors like the severity of the infection, underlying health conditions, and genetic predisposition. However, recognizing this potential link allows for proactive management and preventative measures – such as supporting gut health during and after antibiotic treatment (more on that later) – to minimize dermatological consequences.
Gut Health & The Skin-Gut Axis
The relationship between the gut microbiome and skin health, often referred to as the skin-gut axis, is increasingly recognized in dermatology. A healthy gut microbiome contributes to a strong immune system and reduced systemic inflammation, both crucial for maintaining skin barrier function and preventing flare-ups. UTIs and their treatment – particularly antibiotic use – can significantly disrupt this delicate balance. – Antibiotics are indiscriminate; they kill both harmful bacteria and beneficial ones residing in the gut. This disruption leads to dysbiosis: an imbalance in the gut microbiome.
Dysbiosis is associated with increased intestinal permeability, often called “leaky gut”. When the gut lining becomes more permeable, it allows undigested food particles and bacterial toxins to enter the bloodstream, further fueling inflammation and potentially triggering immune responses that affect the skin. This can manifest as acne, eczema flare-ups, or other inflammatory skin conditions. The connection is bidirectional; a compromised skin barrier can also influence the gut microbiome, creating a feedback loop. A weakened skin barrier allows for increased exposure to allergens and pathogens, which can exacerbate inflammation both locally (on the skin) and systemically (in the gut).
Restoring gut health after antibiotic treatment is therefore vital not only for overall wellbeing but also for minimizing dermatological complications. Strategies include consuming probiotic-rich foods (yogurt, kefir, sauerkraut), incorporating prebiotics into your diet (foods that feed beneficial bacteria like garlic, onions, and bananas), and considering a probiotic supplement under the guidance of a healthcare professional. A diversified diet rich in fiber is also crucial to support a healthy gut microbiome.
Managing Skin Conditions During & After UTIs
If you’re prone to skin conditions and frequently experience UTIs, proactive management can significantly reduce flare-ups. First and foremost, prioritize prevention – staying well hydrated, practicing good hygiene, and addressing any underlying factors that increase your UTI risk are crucial steps. When a UTI does occur: 1. Focus on hydration: Drinking plenty of water helps flush out bacteria and supports overall health. 2. Support gut health: As discussed earlier, consider probiotics and prebiotic-rich foods during and after antibiotic treatment. 3. Minimize stress: Stress can exacerbate both UTIs and skin conditions; incorporate relaxation techniques like meditation or yoga into your routine.
For existing skin conditions, adjust your skincare routine as needed. During a UTI flare-up: – Use gentle, fragrance-free cleansers and moisturizers to avoid irritating already sensitive skin. – Avoid harsh exfoliants or active ingredients that might further compromise the skin barrier. – Consider applying soothing emollients like colloidal oatmeal or shea butter to reduce inflammation and redness. If you notice your skin condition worsening significantly during a UTI, don’t hesitate to consult with a dermatologist. They can provide personalized advice and adjust your treatment plan accordingly.
The Role of Inflammation & Antioxidants
Inflammation is at the core of the connection between UTIs and skin conditions. While the immune response is necessary for fighting infection, chronic or excessive inflammation can damage tissues and exacerbate symptoms. Antioxidants play a vital role in neutralizing free radicals – unstable molecules that contribute to inflammation and oxidative stress. Incorporating antioxidant-rich foods into your diet can help mitigate these effects. – Berries (blueberries, strawberries) – Leafy green vegetables (spinach, kale) – Nuts and seeds – Green tea
Beyond dietary sources, topical antioxidants like vitamin C and E can also be beneficial for skin health. These ingredients help protect the skin barrier, reduce inflammation, and promote collagen production. However, it’s crucial to choose products formulated with stable forms of these vitamins to ensure their effectiveness. Remember that managing inflammation isn’t just about combating the immediate effects of a UTI; it’s about adopting a lifestyle that supports overall health and resilience. This includes getting adequate sleep, managing stress levels, and engaging in regular physical activity.
When To Seek Professional Advice
While this article explores the interconnectedness between UTIs and skin conditions, it’s important to emphasize that it is not intended as medical advice. If you suspect a UTI, consult with your healthcare provider for proper diagnosis and treatment. Similarly, if you experience significant changes in your skin condition – especially during or after a UTI – seek guidance from a dermatologist. Here are some red flags to watch out for: – Severe or persistent skin rash – Widespread hives or itching – Signs of infection (pus, redness, swelling) on the skin – Sudden worsening of existing skin conditions
Don’t attempt to self-diagnose or treat these issues; professional evaluation is essential. Your healthcare team can help determine the underlying cause of your symptoms and develop a personalized treatment plan that addresses both the UTI and any associated dermatological concerns. Remember, holistic care – addressing the interconnectedness between different body systems – often leads to the most effective and sustainable outcomes.