Chronic cystitis, often referred to as interstitial cystitis/bladder pain syndrome (IC/BPS), is a complex condition characterized by persistent bladder discomfort, pelvic pain, and urinary frequency/urgency. It’s far more than just a simple bladder infection; it’s a chronic inflammatory state where the exact cause remains elusive for many sufferers. The impact extends beyond physical symptoms, often significantly affecting quality of life – impacting sleep, work, relationships, and mental wellbeing. Understanding this condition requires moving beyond traditional definitions of bacterial cystitis and exploring the potential interplay between bladder dysfunction, neuroinflammation, and, crucially, the body’s immune response.
The growing research suggests that IC/BPS isn’t merely a localized problem within the bladder itself but is intricately linked to broader systemic inflammation and potential immune dysregulation. This means that the ongoing inflammatory processes within the bladder could potentially affect how well the entire immune system functions – its ability to respond effectively to infections, heal injuries, and even prevent autoimmune reactions. While research is still evolving, there’s a compelling case for investigating this connection, as it may offer new avenues for understanding the condition and developing more effective treatments. The aim isn’t to diagnose or treat but to explore what current scientific thinking suggests about the relationship between chronic cystitis and immune function.
The Inflammatory Landscape of Chronic Cystitis
Chronic cystitis is fundamentally an inflammatory disease. However, unlike many infections where inflammation resolves once the trigger is removed, in IC/BPS, the inflammation persists. This isn’t necessarily due to a continued bacterial infection (though some individuals may have co-existing low-grade infections), but rather appears to be driven by a complex interplay of factors including:
- Bladder lining defects – allowing irritants to penetrate more easily.
- Autoimmune responses – where the body mistakenly attacks its own bladder tissues.
- Neuroinflammation – inflammation of the nerves within the bladder wall, amplifying pain signals.
- Mast cell activation – releasing inflammatory mediators that contribute to symptoms.
The persistent nature of this inflammation is key. Chronic inflammation can exhaust the immune system, diverting resources away from other necessary functions. This means the body has less “reserve” capacity when faced with new threats like viral infections or injuries. It’s akin to constantly running a marathon – eventually, you deplete your energy stores and become more vulnerable. The exact mechanisms of this depletion are still under investigation, but it’s believed that chronic inflammation leads to altered immune cell activity and reduced production of key immune molecules.
The type of inflammation also matters. In IC/BPS, the inflammatory response often involves a shift towards Th2 dominance. This means an overactivation of T helper 2 cells, which are associated with allergic reactions and antibody production. While Th2 responses are important for combating parasites, they can also contribute to chronic inflammation and potentially exacerbate autoimmune processes. The imbalance between different types of immune responses – Th1, Th2, and others – is a hallmark of many chronic inflammatory conditions, and IC/BPS appears to follow this pattern. This shift isn’t always present in every individual with IC/BPS but has been observed in significant studies.
Potential Systemic Effects & Immune Dysregulation
The localized inflammation within the bladder doesn’t stay contained. Inflammatory mediators released during cystitis can enter the bloodstream and trigger systemic effects, potentially impacting immune function in several ways. One major consequence is immune activation. The constant presence of inflammatory signals keeps the immune system in a state of heightened alert, even without a real threat. This chronic activation can lead to:
- Increased levels of pro-inflammatory cytokines – signaling molecules that amplify inflammation throughout the body.
- Reduced responsiveness to new infections – as the immune system is already “busy” dealing with the bladder inflammation.
- Increased risk of autoimmune reactions – due to the heightened state of immune arousal and potential for cross-reactivity (where antibodies meant to target bladder tissues mistakenly attack other healthy tissues).
Furthermore, chronic stress associated with persistent pain and urinary symptoms can also suppress immune function. Stress hormones like cortisol, while initially helpful in short bursts, can become detrimental when chronically elevated. They impair the activity of natural killer cells – crucial for fighting off viruses and cancer cells – and reduce the production of antibodies. This creates a vicious cycle where inflammation leads to stress, which further suppresses the immune system, exacerbating the underlying condition. The interplay between psychological stress and immune function is well-documented in other chronic illnesses and likely plays a significant role in IC/BPS as well.
Impact on Gut Health & Microbiome
A crucial aspect often overlooked is the gut microbiome’s role. The gut harbors trillions of bacteria that play a vital part in immune regulation. A healthy gut microbiome helps “train” the immune system to distinguish between friend and foe, preventing overreactions and maintaining tolerance to self-tissues. Chronic inflammation, like that experienced in IC/BPS, can disrupt this delicate balance, leading to:
- Dysbiosis – an imbalance in the gut bacteria composition.
- Increased intestinal permeability (“leaky gut”) – allowing inflammatory molecules and toxins to enter the bloodstream.
- Impaired immune cell development – as the gut is a major site for immune cell maturation.
Studies suggest individuals with IC/BPS often have altered gut microbiome profiles compared to healthy controls. This dysbiosis can further fuel systemic inflammation, creating a feedback loop that worsens both bladder symptoms and overall immune function. Restoring gut health through dietary changes (like reducing processed foods and increasing fiber intake), probiotics, or prebiotics may be a potential strategy for modulating the immune response in IC/BPS, although more research is needed.
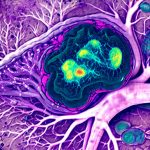
The Role of Mast Cells & Neuroinflammation
Mast cells are key players in both allergy responses and chronic inflammation. In IC/BPS, mast cells appear to be hyperactive within the bladder wall, releasing histamine and other inflammatory mediators that contribute to pain and urinary symptoms. This hyperactivity isn’t always IgE-mediated (like typical allergies); it can also be triggered by non-allergic stimuli like stress or changes in temperature. Chronic activation of mast cells leads to a sustained release of inflammatory molecules, further contributing to systemic inflammation and potentially impacting immune function.
Neuroinflammation – inflammation within the nervous system – is another emerging area of research. The bladder nerves become sensitized during chronic cystitis, leading to amplified pain signals. This neuroinflammation isn’t just a consequence of bladder dysfunction; it can also actively contribute to the inflammatory process itself. Inflammatory mediators released from mast cells and other immune cells can directly affect nerve function, creating a positive feedback loop that exacerbates both pain and inflammation. Furthermore, neuroinflammation has been linked to altered immune cell activity in other chronic pain conditions, suggesting a potential connection with IC/BPS.
Future Directions & Research Needs
Understanding the precise relationship between chronic cystitis and overall immune function is an ongoing process. Current research is focused on:
- Identifying specific biomarkers – measurable indicators of inflammation and immune activation – that can help diagnose and monitor disease progression in IC/BPS.
- Investigating the role of different immune cell subtypes – beyond just Th1 and Th2 cells – to gain a more nuanced understanding of the immune response.
- Developing targeted therapies – aimed at modulating specific aspects of the immune system, such as reducing mast cell activation or restoring gut microbiome balance.
It’s crucial to remember that self-treating or attempting to diagnose based on this information is not advisable. Individuals experiencing chronic cystitis symptoms should seek evaluation and guidance from a qualified healthcare professional. The future of IC/BPS treatment likely lies in a more holistic approach – addressing both the bladder dysfunction and the underlying immune dysregulation, potentially leading to improved outcomes and quality of life for those affected by this challenging condition. Further research is essential to unlock the complexities of this relationship and develop effective, personalized treatments.