Prostatitis is a complex condition encompassing a range of inflammatory and non-inflammatory prostate disorders that can cause significant discomfort and impact quality of life for many men. Traditional understandings have largely focused on bacterial infection, autoimmune responses, or nerve damage as primary drivers, but emerging research suggests a more nuanced picture may be developing. Increasingly, attention is being directed towards the potential role of mast cells—immune cells central to allergic reactions and inflammation—in the pathology of various prostatitis subtypes.
This exploration delves into the growing evidence linking mast cell activation with prostatitis symptoms, examining how these cells function within the prostate environment and discussing possible implications for diagnosis and future therapeutic strategies. It is important to note that this remains an area of ongoing investigation, and much more research is needed to fully understand the relationship between mast cells and the diverse manifestations of prostatitis.
The Immune Landscape of Prostatitis
Prostatitis isn’t a single disease entity; it’s categorized into acute bacterial prostatitis, chronic bacterial prostatitis, chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), and asymptomatic inflammatory prostatitis. While infection plays a clear role in the acute and some chronic bacterial forms, CP/CPPS—the most common type—often lacks identifiable infectious causes. This has led researchers to explore other contributing factors, including immune dysregulation. The prostate’s unique anatomical location and physiological characteristics contribute to its susceptibility to inflammation.
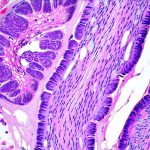
The prostate gland is considered an immunologically privileged site, meaning it normally exhibits reduced immune surveillance. However, this privilege can be disrupted by injury or infection, triggering an inflammatory response involving various immune cells, including mast cells. These cells reside in the prostatic tissue and are capable of releasing a variety of pro-inflammatory mediators that could contribute to the symptoms experienced by men with prostatitis.
Emerging Evidence for Mast Cell Involvement
Recent studies have identified increased numbers of activated mast cells within prostate tissue samples obtained from patients with CP/CPPS compared to healthy controls. This activation is often correlated with symptom severity, suggesting a potential link between mast cell activity and clinical presentation. Furthermore, elevated levels of mast cell mediators like histamine, tryptase, and prostaglandin D2 have been detected in the prostatic fluid and serum of men experiencing prostatitis symptoms, reinforcing this hypothesis.
Mast Cell Function and Mediator Release
Mast cells are granulated immune cells that play a critical role in initiating and modulating inflammatory responses. Upon activation—triggered by various stimuli including pathogens, allergens, neuropeptides or tissue injury – mast cells rapidly release a diverse array of preformed and newly synthesized mediators. These include histamine, tryptase, chymase, prostaglandins, leukotrienes, cytokines, and growth factors. Histamine, for example, increases vascular permeability and causes vasodilation, contributing to swelling and pain. Tryptase is often used as a marker of mast cell activation. Prostaglandins can heighten sensitivity to pain signals. The collective effect of these mediators can significantly contribute to the symptoms associated with prostatitis – pelvic pain, urinary frequency/urgency, and sexual dysfunction.
Potential Triggers for Mast Cell Activation in Prostatitis
Identifying the specific triggers that initiate mast cell activation within the prostate is crucial for understanding the underlying mechanisms driving this condition. Several potential factors have been proposed. Nerve damage or increased sensitivity (neuropathic pain) could directly activate mast cells through neurogenic inflammation, a process where nerve stimulation releases substances that trigger mast cell degranulation. Pelvic floor dysfunction and related muscle tension may also contribute to mechanical stress on the prostate, leading to activation. Furthermore, low-grade infections, even those not detectable by standard methods, or autoimmune responses could provide ongoing stimuli for mast cell activation. Dietary factors and gut health are being explored as potential contributors too, given their impact on systemic inflammation.
Implications for Diagnosis and Treatment
If mast cell activation is indeed a significant driver in many cases of CP/CPPS, it opens up new avenues for both diagnosis and treatment. Currently, diagnosing prostatitis relies heavily on symptom assessment, physical examination, and laboratory tests to rule out bacterial infection. Incorporating biomarkers reflecting mast cell activation—such as levels of histamine or tryptase in prostatic fluid or serum – could potentially improve diagnostic accuracy and help identify patients who might benefit from targeted therapies. Therapeutic strategies aimed at stabilizing mast cells or blocking their mediators are being investigated. These include medications like antihistamines, mast cell stabilizers (cromolyn sodium), and leukotriene inhibitors. However, it’s important to stress that these approaches are still largely experimental in the context of prostatitis, and more rigorous clinical trials are needed to establish their efficacy and safety. Further research is also focused on understanding individual patient variations in response to different treatment strategies, recognizing that prostatitis is a heterogeneous condition.
The exploration of mast cell activation in prostatitis represents an exciting area of investigation with the potential to significantly improve our understanding and management of this challenging condition. While much remains to be discovered, the growing body of evidence suggests that these cells play a more substantial role than previously recognized. Future research will need to focus on unraveling the complex interplay between mast cells, other immune cells, the nervous system, and the prostate microenvironment to develop targeted therapies that effectively address the underlying mechanisms driving prostatitis symptoms and improve the quality of life for affected individuals.