Chronic pain is a complex and debilitating condition affecting millions worldwide. While often attributed to physical injury or underlying disease, emerging research suggests environmental factors play a significant role in modulating pain perception and intensity. Among these factors, changes in atmospheric pressure are increasingly recognized as potential contributors to fluctuations in chronic pain symptoms. Understanding the relationship between barometric pressure and pain can empower individuals living with chronic conditions to better manage their experiences and potentially mitigate some of their challenges.
The link isn’t always straightforward; it involves intricate interactions between physiological systems and environmental stimuli. Many people report noticeable increases in pain levels before inclement weather, particularly during drops in atmospheric pressure associated with storms or changing weather patterns. This observation has prompted scientific investigation into the mechanisms that might explain this phenomenon, moving beyond anecdotal evidence to explore the biological basis for these experiences.
The Science of Atmospheric Pressure and Pain Perception
Atmospheric pressure refers to the weight of air above a given point. It constantly fluctuates due to various meteorological events, including changes in temperature, altitude, and weather systems. These shifts can impact human physiology in several ways, potentially influencing pain perception. Variations in air pressure don’t merely affect those with existing conditions; they can also influence healthy individuals, though the effects are typically more pronounced in those already experiencing chronic discomfort.
The exact mechanisms linking atmospheric pressure to chronic pain remain a subject of ongoing research, but current theories point towards several interconnected physiological processes. These include alterations within the nervous system, inflammatory responses, and changes in tissue fluid dynamics.
How Pressure Changes Affect the Body
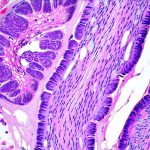
Changes in atmospheric pressure can affect various bodily systems, contributing to fluctuations in pain levels. One key area is the impact on tissues and joints. Lower air pressure allows tissues to expand, potentially irritating sensitive nerve endings and exacerbating existing inflammation. This effect is particularly relevant for individuals with conditions like arthritis or fibromyalgia. Additionally, pressure changes can influence fluid balance within the body, affecting joint lubrication and increasing discomfort.
The Role of Inflammation
Inflammation is a central component in many chronic pain conditions. Fluctuations in atmospheric pressure may modulate inflammatory processes within the body. Some research suggests that falling barometric pressure can trigger an increase in pro-inflammatory cytokines – signaling molecules involved in inflammation – potentially leading to heightened pain sensitivity and symptom flares. This isn’t necessarily about causing new inflammation, but rather amplifying existing, underlying inflammatory responses.
The connection between atmospheric pressure and inflammation is still being actively investigated. It’s thought that the body perceives these pressure changes as a kind of stressor, activating immune responses and leading to increased levels of inflammatory markers. This can create a vicious cycle where pain intensifies due to inflammation triggered or exacerbated by barometric shifts.
Nerve Sensitivity and Pain Pathways
Chronic pain often involves altered nerve function and sensitization, meaning that nerves become more easily activated and respond disproportionately to stimuli. Atmospheric pressure changes may further contribute to this sensitization. Some theories propose that pressure fluctuations can directly impact the functioning of nociceptors – sensory neurons responsible for detecting pain signals – making them more reactive.
This heightened sensitivity can lead to a phenomenon known as allodynia, where normally non-painful stimuli are perceived as painful. Even gentle touch or minor movements can become excruciating when nerve pathways are sensitized by pressure changes and underlying chronic conditions. The interaction between atmospheric pressure fluctuations and these pain pathways is complex and varies among individuals.
Fluid Dynamics and Tissue Expansion
As mentioned earlier, changes in atmospheric pressure directly impact fluid dynamics within the body. Lower pressure causes tissues to expand, which can put stress on joints and surrounding nerves. This effect is especially noticeable in areas prone to swelling or inflammation, such as arthritic joints. The expansion of tissues can also compress nerve endings, triggering pain signals.
Furthermore, fluctuations in air pressure can affect synovial fluid within joints – the lubricating substance that reduces friction between bones. Changes in this fluid’s viscosity and volume may impact joint movement and contribute to discomfort. This interplay between atmospheric pressure, tissue expansion, and fluid dynamics underscores the complex relationship between weather patterns and chronic pain experience.
Ultimately, understanding how changes in atmospheric pressure influence chronic pain is an evolving area of research. It’s important for individuals experiencing these fluctuations to track their symptoms alongside weather patterns to identify personal sensitivities and develop coping strategies. While we cannot control the weather, acknowledging its potential impact on pain perception can empower us to better manage our conditions and advocate for individualized care plans. Focusing on holistic approaches that address both physical and environmental factors may offer the most effective path towards improved well-being for those living with chronic pain.