The intricate connection between diet and bladder symptoms is often underestimated, yet it’s deeply rooted in cellular processes. Many individuals experience frustrating bladder issues – urgency, frequency, pain, incontinence – that may seem unrelated to what they eat. However, the reality is far more complex. What we consume directly impacts the health and functionality of our bladder cells, influencing inflammation, nerve sensitivity, and overall bladder capacity. This isn’t merely about avoiding obvious irritants like caffeine or alcohol; it’s about understanding how specific dietary components interact with cellular pathways to either exacerbate or alleviate these symptoms.
The human body is a network of interconnected systems, and the urinary system is no exception. Dietary choices influence systemic inflammation, gut health (which has a bidirectional relationship with bladder function), and even the production of neurotransmitters that affect bladder control. Ignoring this interplay can lead to chronic discomfort and diminished quality of life. This article will explore these connections on a cellular level, detailing how different foods and dietary patterns impact bladder cells and contribute to symptom development or relief, moving beyond superficial recommendations to understand the why behind dietary interventions.
Dietary Components & Bladder Cell Function
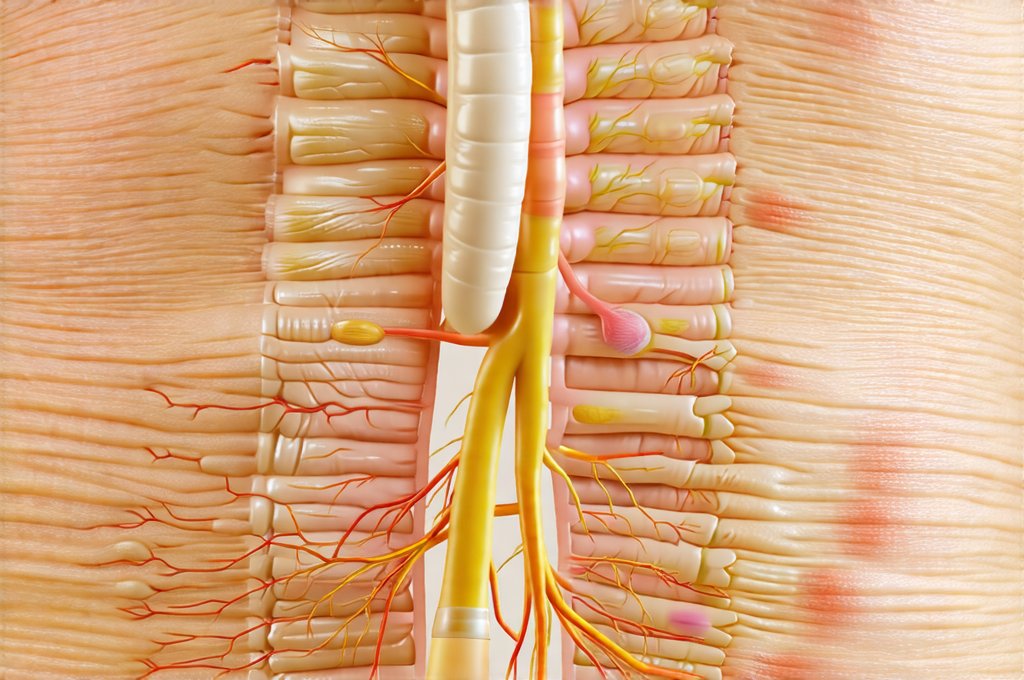
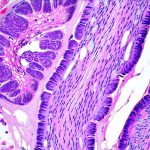
Bladder cells, like all cells in the body, require specific nutrients to function optimally. A diet lacking essential vitamins, minerals, and antioxidants can compromise cellular integrity and increase susceptibility to damage. Specifically, the urothelium – the specialized lining of the bladder – is constantly exposed to urine, making it vulnerable to irritation and inflammation. Certain dietary components directly impact this sensitive layer. For example, diets high in processed foods, sugar, and unhealthy fats promote chronic low-grade inflammation throughout the body, including within the urinary tract. This inflammation damages urothelial cells, increasing their sensitivity and triggering symptoms like urgency and pain. Conversely, a diet rich in anti-inflammatory foods – such as fruits, vegetables, and omega-3 fatty acids – can protect these cells and reduce inflammation. Learning how to improve bladder health through diet and habits is a great first step towards managing symptoms.
The permeability of the bladder lining is also influenced by dietary fat composition. Diets high in saturated and trans fats increase urothelial permeability, making it easier for irritants to penetrate the bladder wall and trigger symptoms. This effect has been demonstrated in studies examining the link between dietary fat intake and interstitial cystitis/bladder pain syndrome (IC/BPS). Furthermore, gut health plays a pivotal role; an imbalance of gut bacteria (dysbiosis) can lead to increased intestinal permeability (“leaky gut”), allowing inflammatory molecules to enter the bloodstream and reach the bladder. Dietary fiber is crucial for maintaining a healthy gut microbiome and reducing inflammation.
Finally, certain foods contain compounds that directly irritate the bladder. These are often individualized – what triggers one person may not affect another – but common culprits include caffeine, alcohol, citrus fruits, spicy foods, and artificial sweeteners. The mechanism of irritation varies; some compounds increase nerve sensitivity in the bladder, while others chemically damage urothelial cells. Understanding these individual sensitivities is key to tailoring dietary interventions. A bladder diary can help track triggers and identify patterns.
Cellular Mechanisms & Bladder Irritation
At a cellular level, bladder irritation involves several interconnected pathways. One primary pathway involves the release of inflammatory mediators – cytokines and chemokines – from damaged or irritated urothelial cells. These mediators activate immune cells in the bladder wall, leading to further inflammation and pain. Dietary factors can significantly influence this process. For example, curcumin, found in turmeric, has potent anti-inflammatory properties and can suppress the release of these inflammatory mediators. Similarly, omega-3 fatty acids have been shown to modulate the production of pro-inflammatory cytokines.
Another key mechanism involves nerve sensitization. The bladder is densely innervated with sensory nerves that detect stretch and fullness. Chronic irritation or inflammation can lead to neuroplasticity – changes in the sensitivity of these nerves, resulting in heightened pain perception. This is a common feature of IC/BPS, where even small amounts of urine can trigger intense pain. Certain dietary components, such as capsaicin (found in spicy foods) and histamine (present in fermented foods), can directly activate or sensitize these nerve fibers.
Furthermore, oxidative stress – an imbalance between the production of free radicals and the body’s ability to neutralize them – plays a significant role in bladder irritation. Free radicals damage cellular structures, including urothelial cells and nerve fibers. A diet lacking antioxidants – vitamin C, vitamin E, selenium – increases susceptibility to oxidative stress. Conversely, antioxidant-rich foods protect against this damage and support cellular health.
The Role of the Microbiome
The gut microbiome’s influence extends beyond inflammation; it directly affects bladder function through the production of metabolites that impact neuronal signaling. Specifically, microbial dysbiosis can lead to an overabundance of bacteria that produce compounds like oxalate, which are known bladder irritants. These compounds are absorbed into the bloodstream and excreted by the kidneys, concentrating in the urine and irritating the bladder lining. A healthy microbiome, fostered through a diet rich in fiber and fermented foods, reduces the production of these harmful metabolites.
The gut-bladder axis is bidirectional; signals travel both ways. Bladder inflammation can also impact gut health, creating a vicious cycle. For instance, chronic stress associated with bladder pain can alter gut motility and microbial composition. Addressing gut health through dietary interventions – probiotics, prebiotics, elimination diets to identify food sensitivities – can therefore have a profound effect on bladder symptoms.
Antioxidant Defense & Urothelial Integrity
Urothelial cells possess inherent antioxidant defense mechanisms, but these can be overwhelmed by oxidative stress. Dietary antioxidants support these defenses and protect the bladder lining from damage. Vitamin C is particularly important for urothelial health; it’s concentrated in the bladder wall and acts as a scavenger of free radicals. Similarly, vitamin E protects cell membranes from lipid peroxidation – a process that damages cellular integrity.
Beyond vitamins, certain plant compounds – polyphenols found in berries, green tea, and dark chocolate – have potent antioxidant and anti-inflammatory properties. These compounds can modulate cellular signaling pathways to protect urothelial cells from damage and promote repair. Furthermore, sulforaphane, found in broccoli sprouts, activates Nrf2 – a master regulator of antioxidant defense genes.
Dietary Fat & Bladder Permeability
As previously mentioned, dietary fat composition significantly impacts bladder permeability. Saturated and trans fats increase urothelial permeability by disrupting tight junctions – the protein structures that seal gaps between cells. This allows irritants to penetrate the bladder wall more easily, triggering inflammation and pain. Conversely, omega-3 fatty acids strengthen tight junctions and reduce permeability.
The ratio of omega-6 to omega-3 fatty acids is also important; a high omega-6 to omega-3 ratio promotes inflammation. Most Western diets are heavily skewed towards omega-6s, found in vegetable oils and processed foods. Increasing omega-3 intake – through oily fish, flaxseeds, chia seeds, or supplements – can help restore balance and reduce bladder irritation. Additionally, limiting saturated and trans fats is crucial for maintaining urothelial integrity. For people on a urology diet, avoiding food fatigue can be challenging but important for long-term adherence.
It’s important to reiterate that dietary interventions are often individualized. What works for one person may not work for another. Keeping a food diary, identifying triggers, and working with a healthcare professional or registered dietitian can help tailor dietary strategies to specific needs and sensitivities. This isn’t about restrictive dieting; it’s about nourishing the body with foods that support cellular health and promote bladder function.