The bladder, a seemingly simple organ, is actually a complex muscular sac responsible for storing urine until it’s conveniently eliminated. Maintaining its integrity is vital for urinary continence and overall well-being. Unfortunately, various factors – from infection to inflammation, radiation therapy, and even chronic catheterization – can compromise the delicate lining of the bladder, known as the urothelium. Recognizing the early signs of urothelial breakdown is critical, not only for timely intervention but also because subtle changes can often be missed or attributed to other causes, leading to delayed diagnosis and potentially more complex treatment needs. This article aims to provide a comprehensive guide on identifying these indicators, empowering individuals to proactively address potential bladder health concerns.
Understanding that the urothelium isn’t simply a passive barrier is key. It’s an active tissue with remarkable regenerative capabilities, but this capacity has limits. When faced with persistent or severe damage, the urothelium can become fragile and vulnerable, leading to symptoms that range from mild discomfort to debilitating pain and urinary dysfunction. A proactive approach—knowing what to look for and promptly discussing any concerns with a healthcare professional—can significantly improve outcomes and preserve bladder health. It’s important to remember this information is not meant to replace medical advice; it’s intended to educate and encourage informed conversations with your doctor.
Recognizing the Early Warning Signs
The initial indicators of bladder lining breakdown are often subtle and easily overlooked, making early detection challenging. These can manifest as changes in urinary habits or sensations – a heightened urgency, increased frequency, or even discomfort during urination. It’s essential to differentiate these symptoms from common occurrences like drinking too much fluid or having a temporary infection. A persistent change, one that doesn’t resolve quickly and is accompanied by other concerning signs, warrants medical attention. Furthermore, blood in the urine (hematuria), even microscopic amounts detected during routine testing, should never be ignored. It’s a red flag indicating potential damage to the bladder lining or other urinary tract issues. The color of the hematuria can vary – bright red if recent and obvious, or darker, tea-colored if older and present in smaller quantities.
Beyond changes in urination, individuals might experience lower abdominal pain or pressure. This discomfort isn’t necessarily sharp or intense; it could be a dull ache that comes and goes. Sometimes, the pain can radiate to the back or pelvis. It’s crucial not to dismiss this as simply “muscle soreness” or attribute it to other causes without investigating further. Chronic inflammation caused by persistent damage to the urothelium can lead to bladder wall thickening and reduced bladder capacity, exacerbating these symptoms. If you’re experiencing chronic pain, consider learning more about early pelvic signs as well.
Finally, a feeling of incomplete emptying – the sensation that your bladder isn’t fully drained even after urinating – can also be an early sign. This may prompt you to visit the bathroom more frequently, creating a vicious cycle of urgency and discomfort. It’s important to note that these signs are not exclusive to bladder lining breakdown; they can also indicate other conditions like urinary tract infections or overactive bladder. Therefore, a comprehensive medical evaluation is essential for accurate diagnosis and appropriate treatment.
Factors Contributing to Urothelial Damage
Several factors can contribute to the breakdown of the bladder’s protective lining. Radiation therapy, often used in cancer treatment for pelvic region cancers (like prostate, cervical, or rectal cancer), can significantly damage the urothelium due to its inherent cytotoxic effects. Even with careful shielding techniques, some radiation inevitably reaches the bladder, causing inflammation and impairing the tissue’s ability to regenerate. Similarly, chemotherapy drugs used to treat various cancers can also have toxic effects on the bladder lining. Certain chemotherapeutic agents are known to cause hemorrhagic cystitis – inflammation of the bladder with bleeding – as a side effect.
Chronic catheterization, while sometimes necessary for individuals unable to empty their bladder naturally, can also contribute to urothelial damage. The presence of a foreign body irritates the bladder wall and increases the risk of infection, both of which can compromise the lining’s integrity. Long-term use of indwelling catheters is associated with higher rates of bladder dysfunction and an increased risk of developing microscopic hematuria. Additionally, recurrent urinary tract infections (UTIs) can lead to chronic inflammation, weakening the urothelium over time. The frequent cycles of infection and antibiotic treatment further disrupt the natural healing processes within the bladder. Finally, certain autoimmune conditions or inflammatory bowel diseases that affect the pelvic region can indirectly impact bladder health and contribute to urothelial damage.
Identifying Specific Symptoms Associated with Treatment-Related Damage
Radiation and chemotherapy often produce distinct symptom profiles. Patients undergoing radiation therapy may experience acute symptoms during treatment—frequent urination, burning sensations, and even blood in the urine—that gradually subside after treatment completion. However, late effects can develop months or years later, including bladder fibrosis (scarring) leading to reduced capacity and chronic urinary urgency. Chemotherapy-induced cystitis often presents with a more abrupt onset of hematuria, sometimes severe enough to require hospitalization. Symptoms may persist even after stopping chemotherapy, requiring specific interventions like irrigation therapy to flush the bladder and reduce bleeding.
Patients who have undergone long-term catheterization might experience a gradual decline in bladder function, characterized by incomplete emptying, urinary leakage, and recurrent infections. The symptoms can be subtle initially but progressively worsen over time. It’s crucial for these individuals to undergo regular cystoscopies—visual examinations of the bladder using a small camera—to monitor the condition of the urothelium and detect any early signs of damage or inflammation.
Recognizing Symptoms Following Infection
UTIs can often present with typical symptoms like burning during urination, frequent urge to urinate, cloudy urine, and lower abdominal discomfort. However, recurrent UTIs, particularly in individuals with underlying bladder dysfunction or compromised immune systems, can lead to chronic inflammation that damages the urothelium over time. The repeated cycles of infection create a persistent inflammatory response, weakening the tissue’s ability to heal and increasing the risk of developing microscopic hematuria.
The symptoms of recurrent UTIs may become less pronounced with each episode, making it difficult to recognize them as infections. Individuals might attribute these subtle changes to other causes or dismiss them as “just another UTI.” It’s important to seek medical attention if you experience frequent urinary symptoms, even if they are mild, to prevent further damage to the bladder lining. In some cases, understanding early stages of bladder spasms can help identify an underlying issue.
The Importance of Cystoscopy and Further Testing
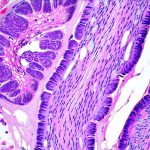
If a healthcare professional suspects urothelial breakdown based on your symptoms and medical history, further investigation is typically required. Cystoscopy, as mentioned earlier, is often the gold standard for evaluating the bladder lining. It allows direct visualization of the bladder wall, enabling identification of inflammation, ulcers, or abnormal growths. Biopsies can be taken during cystoscopy to determine the underlying cause of any abnormalities and rule out more serious conditions like bladder cancer.
Other diagnostic tests may include urine cytology—examining urine samples for abnormal cells—and imaging studies like CT scans or MRIs to assess the extent of damage and identify any associated structural changes. Urodynamic testing, which measures bladder function during filling and emptying, can help evaluate bladder capacity, flow rates, and overall urinary dynamics. If you’re concerned about potential stones, it is important to know first signs of bladder stones in women. A comprehensive evaluation is essential for accurate diagnosis and development of a personalized treatment plan tailored to your specific needs. Additionally, you may want to learn how to support the bladder naturally every day.
It’s vital to reiterate that this information should not be used as a substitute for professional medical advice. If you are concerned about your bladder health or experiencing any of the symptoms described above, please consult with a healthcare provider for proper evaluation and guidance.