Chronic cystitis, often characterized by persistent bladder pain and urinary frequency, is a frustrating condition for many individuals. The symptoms can significantly impact quality of life, leading to sleep disturbances, emotional distress, and difficulties with daily activities. While traditionally understood as an inflammatory response to bacterial infection – acute cystitis being the typical example – chronic cystitis frequently persists despite negative urine cultures, prompting researchers and clinicians to explore alternative underlying mechanisms. This has led to growing interest in whether this persistent form of bladder dysfunction could be linked to autoimmune processes, where the body’s immune system mistakenly attacks its own tissues.
The complexity arises because diagnosing chronic cystitis itself can be challenging. Often, it’s grouped under broader terms like Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS), a diagnosis of exclusion meaning other causes must first be ruled out. This diagnostic ambiguity complicates research into the condition’s etiology and potential treatment strategies. The lack of definitive biomarkers also makes it difficult to pinpoint specific disease mechanisms, fueling ongoing debate about whether autoimmune pathways are truly involved or if other factors—like nerve damage, mast cell activation, or myofascial pain—are more central to the development of chronic symptoms. Understanding these complexities is crucial when considering the possibility of an autoimmune link.
The Autoimmune Hypothesis and IC/BPS
The idea that chronic cystitis (or IC/BPS) could have an autoimmune component isn’t new, but it’s gaining traction with advances in immunological research. Several lines of evidence support this hypothesis. Firstly, there is a higher prevalence of autoimmune diseases among individuals diagnosed with IC/BPS compared to the general population. Conditions like Sjögren’s syndrome, Lupus, and Hashimoto’s thyroiditis are observed more frequently in these patients, suggesting a potential genetic predisposition or shared immunological vulnerabilities. This isn’t to say that having one autoimmune disease causes IC/BPS, but it hints at an underlying immune dysregulation.
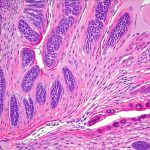
Secondly, studies have shown evidence of immune cell infiltration within the bladder wall of individuals with chronic cystitis. Specifically, T cells, mast cells, and natural killer (NK) cells are often found in increased numbers in biopsies from affected patients. These immune cells release inflammatory cytokines – signaling molecules that promote inflammation—potentially contributing to the ongoing pain and discomfort experienced by those with chronic symptoms. The specific types of cytokines identified also suggest an autoimmune response; for example, elevated levels of interferon gamma, a cytokine associated with cell-mediated immunity, have been observed in bladder tissue samples.
Finally, some research indicates the presence of autoantibodies – antibodies that target the body’s own tissues—in patients with IC/BPS. While identifying consistent and reliable autoantibody targets has proven difficult (and remains an area of ongoing research), the detection of these antibodies suggests the immune system is misdirected against bladder wall components, potentially initiating and perpetuating inflammation. The exact role these autoantibodies play in disease pathogenesis is still being investigated, but their presence lends further support to the autoimmune hypothesis.
Exploring Immune Dysregulation in Chronic Cystitis
Beyond the basic evidence for autoimmunity, researchers are delving into specific mechanisms of immune dysregulation that may be at play in chronic cystitis. One key area of focus is mast cell activation. Mast cells are immune cells involved in allergic reactions and inflammation, and they’re found in abundance within the bladder wall. In individuals with IC/BPS, these mast cells appear to be hyper-reactive, releasing histamine and other inflammatory mediators even without a clear trigger. This chronic mast cell activation can lead to increased bladder sensitivity, pain, and urgency.
Another avenue of investigation centers on the role of the epithelial barrier within the bladder. A healthy bladder lining acts as a protective barrier against harmful substances in urine. In IC/BPS, this barrier often becomes compromised – “leaky” – allowing potentially irritating compounds to penetrate deeper into the bladder wall and trigger an immune response. This breakdown in barrier function may be caused by inflammation or genetic predispositions and can lead to a vicious cycle of irritation, inflammation, and further barrier damage.
Furthermore, there’s growing recognition that neuroinflammation—inflammation within the nervous system—plays a role in chronic cystitis symptoms. The bladder is richly innervated with nerve fibers, and chronic inflammation can sensitize these nerves, leading to pain even in the absence of obvious tissue damage. This neuroinflammation may be triggered by immune cell activity or direct damage to nerve fibers, further blurring the lines between autoimmune and neurological components of the disease.
Diagnostic Challenges & Biomarker Research
Diagnosing IC/BPS, and therefore assessing its potential autoimmune nature, is notoriously difficult. Currently, diagnosis relies heavily on symptom criteria – ruling out other causes like urinary tract infections—and often involves invasive procedures such as cystoscopy with biopsy. This can lead to delayed diagnoses and frustration for patients. There’s a desperate need for reliable biomarkers – measurable indicators of disease activity—to aid in early detection and monitor treatment response.
Researchers are actively searching for these biomarkers, focusing on several areas:
1. Identifying specific autoantibodies that consistently appear in IC/BPS patients. This is challenging due to the heterogeneity of the condition but remains a primary focus.
2. Analyzing cytokine profiles in urine or bladder tissue samples to identify patterns indicative of immune activation and inflammation.
3. Investigating genetic markers associated with increased susceptibility to autoimmune diseases, potentially providing clues about underlying immunological vulnerabilities.
The development of accurate biomarkers would not only improve diagnosis but also help personalize treatment approaches, tailoring therapies to the specific immunological mechanisms driving each patient’s symptoms.
The Role of Immunomodulatory Therapies
If chronic cystitis is indeed linked to autoimmune processes, then immunomodulatory therapies—treatments that alter the immune system—could potentially offer a more targeted approach than current symptomatic treatments. Several immunomodulatory agents are being explored for IC/BPS:
– Low-dose naltrexone (LDN), an opioid receptor antagonist, has shown promise in reducing inflammation and pain by modulating immune cell activity.
– Pentosan polysulfate sodium (PPS) is a drug originally developed as a blood thinner but found to have anti-inflammatory effects within the bladder; its mechanism of action isn’t fully understood but may involve restoring epithelial barrier function.
– Immunosuppressants like methotrexate or cyclosporine, typically used in other autoimmune conditions, are being investigated for severe cases of IC/BPS refractory to conventional treatments, although their use is controversial due to potential side effects.
It’s crucial to understand that these therapies are still largely experimental and should only be considered under the guidance of a qualified healthcare professional. The effectiveness of immunomodulatory approaches varies greatly among individuals, highlighting the complexity of the condition and the need for personalized treatment strategies.
Future Directions in Research
The autoimmune hypothesis in chronic cystitis is far from definitively proven, but it represents a promising avenue for research and potential therapeutic breakthroughs. Future studies should focus on:
– Large-scale epidemiological investigations to determine the prevalence of autoimmune diseases among IC/BPS patients and identify genetic risk factors.
– Longitudinal studies tracking immune cell activity and cytokine levels in bladder tissue over time to understand disease progression and treatment response.
– Developing more sophisticated animal models that accurately mimic the immunological features of human IC/BPS, allowing for rigorous testing of potential therapies.
Ultimately, a deeper understanding of the interplay between immunity, inflammation, and neurological factors will be essential to unraveling the complexities of chronic cystitis and developing effective treatments that address the root causes of this debilitating condition, rather than just managing its symptoms. The pursuit of these answers offers hope for improving the lives of millions affected by chronic bladder pain and urinary dysfunction.