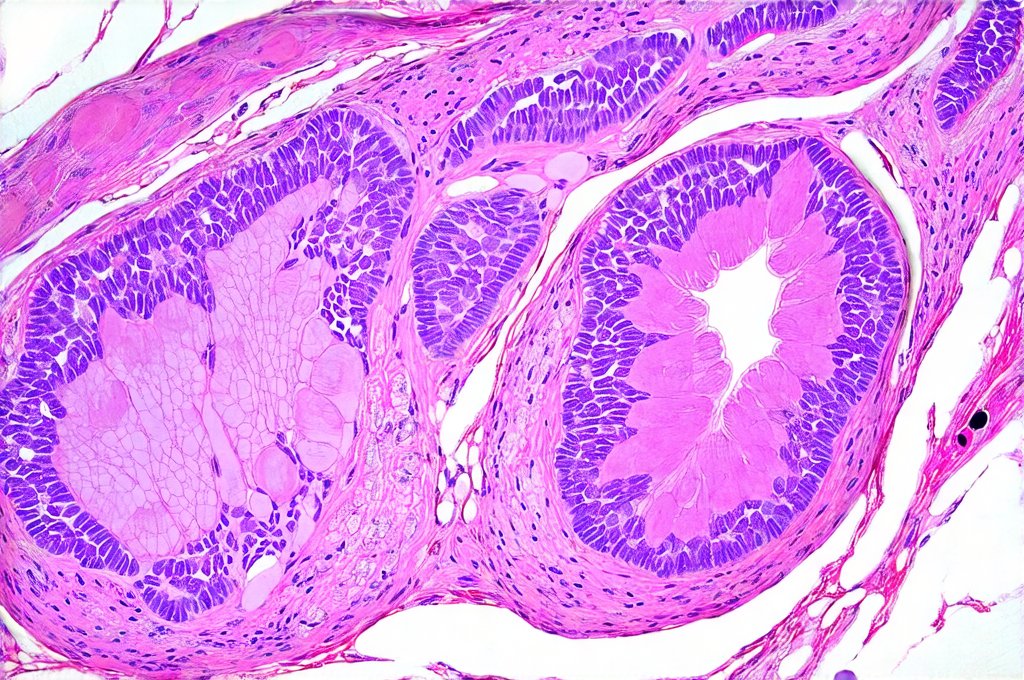
The prostate gland, often discussed in relation to aging men’s health, is a small but vital component of the male reproductive system. Its primary function involves fluid production contributing to semen, aiding in sperm viability and transport. However, this region can be prone to various issues, many stemming from – or significantly impacted by – the intricate network of microcirculation that sustains it. Understanding how blood flow at the capillary level influences prostate health is crucial for grasping both preventative measures and potential treatment strategies. A healthy microcirculation ensures adequate oxygen and nutrient delivery while efficiently removing metabolic waste products; disruptions in this delicate balance can lead to inflammation, tissue damage, and ultimately contribute to a range of prostatic conditions.
Microcirculation, often overlooked, represents the final stage of blood flow – where arteries transition into capillaries and deliver essential resources directly to tissues. In the prostate area, this network is particularly dense due to the gland’s high metabolic activity. Factors like age, lifestyle choices (diet, exercise), underlying health conditions such as diabetes or hypertension, and even chronic inflammation can compromise microcirculatory function. When blood flow becomes restricted, it creates a cascade of negative effects: reduced tissue oxygenation (hypoxia), buildup of waste products, impaired immune response, and increased susceptibility to cellular damage. This compromised environment not only exacerbates existing prostate problems but also paves the way for new ones to develop.
The Role of Microcirculation in Prostatic Hyperplasia (BPH)
Benign prostatic hyperplasia, or BPH, is arguably the most common prostate issue affecting men as they age. While its exact cause isn’t fully understood, there’s a growing body of evidence linking impaired microcirculation to its development and progression. – Chronic inflammation, often present in aging tissues, leads to capillary damage and reduced blood flow. This creates a vicious cycle where hypoxia further fuels inflammation and tissue remodeling. – Reduced oxygen delivery can also lead to changes in the prostate’s cellular environment, promoting the overgrowth of prostatic cells characteristic of BPH. – The constriction of capillaries impedes nutrient supply, weakening tissues and reducing their ability to repair themselves.
The microvascular changes aren’t merely a consequence of BPH; they actively contribute to its symptoms. As blood flow diminishes, the prostate becomes less efficient at eliminating metabolic waste products, leading to swelling and further compression of the urethra. This results in the typical urinary symptoms associated with BPH: frequent urination, difficulty starting or stopping urination, weak urine stream, and nighttime awakenings. Addressing microcirculatory dysfunction alongside conventional BPH treatments may offer a more comprehensive approach to managing the condition and improving quality of life for affected individuals. Research is ongoing to explore therapies specifically targeting microcirculation enhancement in this context, with promising early results suggesting benefits from interventions like targeted exercise programs and specific nutritional supplements. Considering flow patterns could also be beneficial here.
Microcirculation & Prostatitis: A Complex Relationship
Prostatitis, inflammation of the prostate gland, presents differently than BPH, often causing acute or chronic pain in the pelvic region, urinary difficulties, and sometimes sexual dysfunction. The link between microcirculation and prostatitis is particularly complex – it’s both a cause and a consequence of inflammation. – Impaired blood flow weakens the prostate’s immune defenses, making it more vulnerable to infection (in cases of bacterial prostatitis) or inflammatory responses triggered by other factors. – Inflammation itself further damages capillaries, creating a feedback loop that exacerbates microcirculatory dysfunction and perpetuates pain and discomfort. – In chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), which lacks identifiable infectious causes, microcirculation abnormalities are believed to play a significant role in the ongoing pain mechanisms.
The diminished blood flow in chronic cases can lead to localized hypoxia and accumulation of inflammatory mediators, sensitizing nerve endings and contributing to persistent pain even in the absence of active inflammation. Treatment strategies for prostatitis often focus on antibiotics (for bacterial forms), anti-inflammatory medications, and pain management. However, integrating therapies aimed at restoring microcirculatory health – such as pelvic floor exercises, lifestyle modifications promoting blood flow, and potentially pharmacological interventions – could offer a more holistic approach to alleviating symptoms and improving long-term outcomes. If you experience discomfort in the urethral area, seek medical advice.
The Impact of Lifestyle Factors on Prostate Microcirculation
Numerous lifestyle factors significantly influence prostate microcirculation: – Diet: A diet rich in antioxidants (fruits, vegetables) helps protect capillaries from damage while reducing inflammation. Conversely, diets high in processed foods, saturated fats, and sugar can impair blood flow and promote inflammatory processes. – Exercise: Regular physical activity improves overall cardiovascular health, enhancing blood circulation throughout the body, including the prostate region. Specific exercises targeting the pelvic floor muscles (Kegels) can directly improve microcirculation to the prostate. – Stress Management: Chronic stress elevates cortisol levels, which can constrict blood vessels and impair microcirculatory function. Techniques like meditation, yoga, or deep breathing exercises help reduce stress and promote healthy blood flow.
Maintaining a healthy weight is also crucial, as obesity contributes to systemic inflammation and impairs vascular health. Avoiding smoking is paramount, as nicotine damages capillaries and reduces oxygen delivery. Hydration plays a vital role; adequate water intake ensures optimal blood viscosity and facilitates efficient circulation. These lifestyle modifications represent proactive steps individuals can take to support prostate health and potentially prevent or mitigate microcirculation-related issues. It’s also important to consider if bladder issues run in families.
Potential Therapeutic Interventions for Microcirculatory Enhancement
While research is ongoing, several therapeutic interventions show promise in enhancing prostate microcirculation: – Pharmacological Approaches: Certain medications, such as pentoxifylline (a hemorrheologic agent) and some vasodilators, can improve blood flow by reducing blood viscosity or dilating capillaries. However, their use requires careful evaluation due to potential side effects and interactions with other medications. – Physical Therapy: Pelvic floor muscle exercises (Kegels), biofeedback therapy, and manual therapies can all contribute to improved microcirculation in the prostate area. These techniques strengthen pelvic muscles, release tension, and enhance blood flow.
- Nutritional Supplements: Some supplements, like L-arginine (a precursor to nitric oxide, a potent vasodilator) and omega-3 fatty acids (with anti-inflammatory properties), may support microcirculatory function. However, it’s essential to consult with a healthcare professional before starting any new supplement regimen. Furthermore, emerging therapies such as low-level laser therapy (LLLT) are being investigated for their potential to stimulate cellular regeneration and improve blood flow in prostate tissues. It is vital to understand that these interventions should be considered complementary to – not replacements for – conventional medical treatments prescribed by a qualified healthcare provider.
The Future of Microcirculation Research in Prostate Health
The understanding of the intricate relationship between microcirculation and prostate health is rapidly evolving. Future research will likely focus on: – Developing more sophisticated imaging techniques to visualize and assess microvascular function within the prostate gland, allowing for earlier detection of abnormalities. – Identifying specific biomarkers that indicate microcirculatory dysfunction in prostate tissues, enabling personalized treatment strategies. – Conducting large-scale clinical trials to evaluate the efficacy of novel therapeutic interventions targeting microcirculation enhancement in various prostate conditions.
- Exploring the role of genetics in predisposing individuals to microvascular abnormalities and prostate disease. The integration of artificial intelligence (AI) and machine learning could also accelerate research by analyzing vast datasets and identifying patterns that might otherwise be missed. Ultimately, a deeper understanding of prostate microcirculation will pave the way for more targeted, effective, and personalized approaches to preventing and treating prostatic diseases, improving the quality of life for men worldwide. If you experience warmth felt in the prostate area after bathroom use, consult your doctor.