The sensation of needing to urinate is fundamental to maintaining bodily homeostasis, but for millions, this seemingly simple process can be disrupted by a range of conditions causing urinary frequency, urgency, pain, and even incontinence. Understanding the complex interplay between the nervous system and the bladder – the urinary sensory pathways – is crucial not only for diagnosing these issues but also for developing effective therapeutic interventions. Historically, treatments focused largely on behavioral therapies or broad-spectrum medications with significant side effects. However, a growing appreciation of the intricacies of these pathways has sparked intense research into pharmacological modulation as a more targeted and refined approach to managing urinary dysfunction. This article will explore the current state of knowledge regarding how we can pharmacologically influence these sensory systems to alleviate suffering and improve quality of life for those affected by bladder disorders.
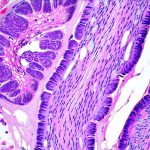
The process begins with stretch receptors within the bladder wall detecting varying degrees of fullness. These signals are then transmitted via afferent nerves – primarily pelvic nerve fibers – to the spinal cord, ultimately reaching higher brain centers responsible for processing sensation and initiating a coordinated response. However, this isn’t simply a one-way street. Descending pathways from the brain can modulate these afferent signals, influencing how fullness is perceived and impacting voiding behavior. Importantly, multiple neurotransmitters and receptors are involved at each stage of this process, offering several potential targets for pharmacological intervention. Disruptions to any point along this pathway – be it altered receptor sensitivity, impaired nerve conduction, or inappropriate central processing – can contribute to the diverse array of urinary symptoms observed in clinical practice.
The Role of Neurotransmitters and Receptors
The bladder’s sensory system relies heavily on a complex network of neurotransmitters. ATP (adenosine triphosphate) is arguably the most important, acting as a co-transmitter with nerves fibers carrying nociceptive signals – those relating to pain. When the bladder stretches, ATP is released, activating P2X receptors located on afferent nerve terminals. These receptors are crucial for initiating the sensation of urgency and contributing to the reflex arc that leads to detrusor contraction. Other key neurotransmitters include CGRP (calcitonin gene-related peptide), which plays a role in modulating bladder sensitivity and potentially enhancing pain perception, and substance P, also involved in nociception and neuroinflammation. Understanding these interactions is paramount for developing targeted therapies.
Pharmacological strategies focusing on these neurotransmitters are showing promise. For example, research into selective P2X receptor antagonists has been ongoing for years, with the aim of reducing bladder urgency without impacting normal voiding function. The challenge lies in achieving sufficient selectivity – many P2X receptors exist throughout the body, and non-selective blockade can lead to unwanted side effects. Similarly, modulating CGRP signaling through antibodies or small molecule inhibitors is being explored as a potential treatment for overactive bladder (OAB) syndromes. Beyond these specific targets, broader approaches focusing on reducing neuroinflammation within the bladder wall – often driven by chronic irritation or infection – are also gaining traction, utilizing anti-inflammatory compounds to dampen afferent nerve activity.
The brain’s role is equally important. Descending modulation from cortical areas and the periaqueductal gray can significantly influence how sensory information from the bladder is interpreted. These descending pathways utilize neurotransmitters like serotonin and norepinephrine, which are also targets for existing medications used in treating conditions like depression and anxiety – explaining why some patients experience improvements in urinary symptoms when treated for comorbid mental health issues. This highlights the intricate connection between psychological state and bladder function, emphasizing a holistic approach to treatment.
Targeting Afferent Nerve Signaling
Pharmacological modulation can directly impact how afferent nerves transmit signals from the bladder to the spinal cord. One strategy involves blocking sodium channels, crucial for nerve impulse generation and propagation. Local anesthetics like lidocaine have been used intravesically (directly into the bladder) to temporarily ‘block’ these channels, reducing sensation and providing symptomatic relief in cases of severe urgency or pain. However, this approach is limited by its transient effect and potential for systemic absorption.
More sophisticated approaches are focusing on developing selective sodium channel blockers with improved pharmacokinetic properties – meaning they can be administered systemically without causing significant side effects. Another target is TRPV1 (transient receptor potential vanilloid 1), a heat-sensitive ion channel expressed on afferent nerve terminals. TRPV1 activation contributes to bladder pain and hypersensitivity, and antagonists are being investigated as potential treatments for interstitial cystitis/bladder pain syndrome (IC/BPS). The challenge here lies in the broad distribution of TRPV1 throughout the body, necessitating careful consideration of selectivity to avoid unwanted effects like altered temperature sensation.
Furthermore, research is exploring neuroprotective strategies aimed at preventing damage to afferent nerve fibers themselves. Chronic bladder irritation can lead to nerve fiber neuropathy, where nerves become damaged and hypersensitive. Compounds with antioxidant properties or those promoting nerve regeneration may offer a longer-term solution for managing chronic pain syndromes associated with urinary dysfunction.
Modulating Spinal Cord Processing
The spinal cord acts as a crucial relay station, processing afferent signals from the bladder before sending them to higher brain centers. Within the spinal cord, glutamate plays a key role in transmitting these signals between neurons. Blocking NMDA receptors – glutamate receptors involved in synaptic plasticity and pain amplification – has been shown to reduce urgency and frequency in animal models of OAB. However, systemic administration of NMDA antagonists can have significant cognitive side effects, limiting their clinical utility.
A more promising approach involves targeting GABAergic interneurons within the spinal cord. GABA is an inhibitory neurotransmitter that helps regulate neuronal activity. Enhancing GABAergic transmission can dampen afferent signals and reduce bladder hyperactivity. Compounds that increase GABA levels or stimulate GABA receptors are being investigated as potential treatments for OAB, offering a more targeted mechanism than broad-spectrum NMDA blockade.
Moreover, the concept of spinal cord neuromodulation is gaining traction. Techniques like electrical stimulation – either percutaneously or via implanted devices – can directly modulate spinal cord activity, influencing voiding behavior and reducing pain perception. While still in its early stages, this approach offers a potentially long-lasting and personalized treatment option for patients with refractory urinary symptoms.
Central Nervous System Targets
The brain plays a crucial role in modulating bladder function, and several central nervous system targets are being explored for pharmacological intervention. As mentioned earlier, neurotransmitters like serotonin and norepinephrine influence descending pathways that can dampen afferent signals and regulate voiding behavior. Selective serotonin reuptake inhibitors (SSRIs) and norepinephrine reuptake inhibitors (NRIs), commonly used to treat depression and anxiety, have shown some benefit in managing OAB symptoms – likely due to their effects on these descending pathways.
However, more targeted approaches are needed. Research is focusing on identifying specific brain regions involved in bladder control and developing compounds that selectively modulate neuronal activity within those areas. For example, the pontine micturition center plays a key role in initiating voiding reflexes, and targeting receptors within this area could potentially restore normal bladder function in patients with neurogenic bladder – where nerve damage disrupts these pathways.
Finally, the emerging field of neuroplasticity offers exciting possibilities. Repeated exposure to pain or discomfort can lead to changes in brain structure and function, contributing to chronic urinary symptoms. Compounds that promote neuroplasticity – helping the brain ‘rewire’ itself – may offer a novel approach to breaking this cycle and restoring normal bladder control. This remains an area of active research, but holds significant promise for developing more effective and long-lasting treatments for urinary dysfunction.