Prostatitis, inflammation of the prostate gland, is a common condition affecting men of all ages, though more prevalent in older demographics. Symptoms can range from mild discomfort to severe pain impacting quality of life, including difficulties with urination, sexual function, and overall pelvic health. Understanding the complexities surrounding prostatitis is crucial, as its causes are often multifaceted and not always clearly defined, leading researchers to explore potential links beyond traditional bacterial infections.
The increasing recognition of autoimmune diseases – conditions where the body’s immune system mistakenly attacks its own tissues – has prompted investigation into their possible role in chronic inflammatory conditions like prostatitis. While traditionally considered a primarily infectious or non-infectious inflammatory condition, emerging evidence suggests that autoimmune processes might contribute to certain forms of persistent prostate inflammation and related symptoms. This article explores the potential connections between prostatitis and autoimmune diseases, examining current research and highlighting areas for further investigation.
Understanding Prostatitis Classifications
Prostatitis isn’t a single disease entity but rather encompasses several distinct clinical syndromes categorized into four main types: acute bacterial prostatitis, chronic bacterial prostatitis, chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), and asymptomatic inflammatory prostatitis. Each type has different underlying causes and treatment approaches. The specific classification significantly impacts the likelihood of an autoimmune connection; bacterial forms are less likely to be directly linked than CP/CPPS which often lacks a clear infectious origin.
The chronic nature of CP/CPPS, characterized by long-term pelvic pain without demonstrable bacterial infection, is where the potential for autoimmune involvement becomes more prominent. The elusive etiology of CP/CPPS has led researchers to consider immune dysregulation as a contributing factor in its development and persistence.
Exploring Autoimmune Disease Characteristics
Autoimmune diseases arise from a breakdown in immunological tolerance – the ability of the immune system to distinguish between self and non-self. This leads to an inappropriate immune response targeting healthy tissues, resulting in chronic inflammation and tissue damage. A vast array of autoimmune conditions exists, including rheumatoid arthritis, lupus, inflammatory bowel disease, and Sjögren’s syndrome, each with unique target organs and clinical manifestations.
The common thread among these diseases is the presence of autoantibodies – antibodies that react against self-antigens – and T cell mediated immune responses targeting the body’s own tissues. Identifying specific autoimmune markers or patterns in individuals with chronic prostatitis could provide valuable insights into this potential connection.
The Role of Autoantibodies in Chronic Prostatitis/CPPS
Research suggests a possible correlation between autoantibody presence and CP/CPPS. Studies have detected various autoantibodies in men experiencing chronic prostate inflammation, including those targeting prostatic tissue itself or components involved in immune regulation. While the presence of autoantibodies doesn’t automatically confirm an autoimmune origin, it indicates that the immune system is reacting to something within the body – potentially misidentifying prostatic tissues as foreign.
However, establishing a causal relationship remains challenging. Autoantibody detection may simply reflect inflammation rather than initiating it. Further research is needed to determine if these autoantibodies play an active role in disease pathogenesis or are merely secondary phenomena resulting from chronic inflammation and tissue damage. Specific antibodies linked to autoimmune conditions like rheumatoid arthritis have also been found at increased levels in some CP/CPPS patients, hinting at potential cross-reactivity or shared immunological mechanisms.
Investigating T Cell Involvement and Cytokine Profiles
T cells, central players in the adaptive immune system, are implicated in the development of many autoimmune diseases. In chronic prostatitis, particularly CP/CPPS, altered T cell populations and cytokine profiles have been observed. Specifically, imbalances between pro-inflammatory (e.g., TNF-alpha, IL-17) and anti-inflammatory cytokines (e.g., IL-10, TGF-beta) may contribute to persistent inflammation.
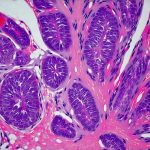
Research indicates that certain T cell subtypes might be more prevalent in the prostate tissue of men with CP/CPPS, suggesting an ongoing immune response. Analyzing these profiles can help identify specific immune pathways driving chronic inflammation and potentially reveal therapeutic targets. The detection of activated T cells within prostatic fluid or tissue biopsies supports the idea of localized immune activation contributing to disease severity.
Potential Overlap with Systemic Autoimmune Conditions
The coexistence of CP/CPPS with established systemic autoimmune diseases isn’t uncommon, raising questions about shared underlying mechanisms. Patients diagnosed with conditions like ankylosing spondylitis, rheumatoid arthritis, or lupus may exhibit a higher incidence of chronic prostatitis symptoms. This overlap suggests that systemic immune dysregulation could predispose individuals to prostate inflammation.
The complex interplay between systemic and localized immune responses requires further investigation. It’s possible that systemic autoimmune diseases exacerbate prostate inflammation or that the inflammatory environment within the prostate can trigger or worsen existing autoimmune conditions elsewhere in the body. Identifying common genetic predispositions or immunological markers across these conditions might provide valuable clues.
Ultimately, the connection between prostatitis and autoimmune diseases remains a complex area of ongoing research. While evidence suggests an immune component in certain forms of chronic prostatitis, particularly CP/CPPS, establishing definitive causal links requires more extensive studies. Further investigations focusing on autoantibody profiles, T cell involvement, cytokine patterns, and epidemiological data will be crucial to unraveling the intricacies of this potential relationship and developing targeted therapies for men experiencing chronic prostate inflammation. A deeper understanding of these connections could revolutionize the approach to diagnosing and treating prostatitis, moving beyond traditional antibacterial strategies to incorporate immunomodulatory interventions where appropriate.