Chronic prostatitis is a complex condition affecting many men, often characterized by persistent pelvic pain, urinary symptoms, and sexual dysfunction. Diagnosing it can be challenging due to overlapping symptoms with other conditions and variations in presentation. While the exact causes remain debated, increasing evidence points towards inflammation as a central driver of the disease process, making understanding the role of inflammatory cytokines crucial for potential therapeutic strategies. This article will delve into the specific cytokines implicated in chronic prostatitis, their sources, mechanisms of action within the prostate, and how they contribute to the development and perpetuation of symptoms.
The inflammatory response is normally protective, but when dysregulated or prolonged, it can become detrimental, causing tissue damage and chronic disease. In chronic prostatitis, this persistent inflammation isn’t always linked to bacterial infection – many cases are classified as non-bacterial chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). This suggests other triggers initiate and maintain the inflammatory cascade, with cytokines acting as key signaling molecules in that process. Identifying these specific cytokines allows for a more targeted approach to understanding disease pathology and potential interventions.
The Role of Inflammation in Chronic Prostatitis
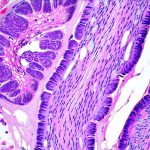
Inflammation is not simply a consequence of chronic prostatitis; it appears to be integral to its development and persistence. It’s now understood that even in cases where bacterial infection isn’t present, an immune response is still activated within the prostate gland, leading to tissue damage and the characteristic symptoms experienced by patients. This suggests autoimmune or autoinflammatory processes may play a role alongside other potential triggers like nerve dysfunction or pelvic floor muscle imbalances.
The prostate’s unique anatomical location and physiological characteristics contribute to its susceptibility to inflammation. Its complex ductal system can become blocked, promoting inflammatory cell accumulation. Furthermore, the blood-prostate barrier, while protecting against infection, also limits immune cell access, potentially leading to a less effective clearance of inflammatory stimuli.
Cytokines as Key Mediators
Cytokines are small signaling proteins that act as messengers between cells of the immune system, orchestrating the inflammatory response. They can be broadly categorized into pro-inflammatory cytokines (promoting inflammation) and anti-inflammatory cytokines (suppressing it). In chronic prostatitis, an imbalance often exists, with a dominance of pro-inflammatory signals contributing to ongoing tissue damage and symptom persistence. Understanding which specific cytokines are elevated in the prostate and surrounding tissues is essential for developing targeted therapies.
Pro-Inflammatory Cytokines: TNF-α & IL-1β
Tumor necrosis factor-alpha (TNF-α) and interleukin-1 beta (IL-1β) are two of the most prominent pro-inflammatory cytokines found elevated in patients with chronic prostatitis. They’re produced by various immune cells like macrophages, neutrophils, and even prostatic epithelial cells themselves, creating a self-amplifying inflammatory loop. TNF-α promotes leukocyte recruitment, vascular permeability, and further cytokine release, while IL-1β contributes to pain sensitization and prostate tissue damage.
These cytokines aren’t just present in the prostate gland itself. Studies have detected increased levels of TNF-α and IL-1β in the seminal fluid and serum of men with chronic prostatitis, suggesting systemic effects beyond localized inflammation within the prostate. This may explain some of the broader symptoms associated with CP/CPPS like fatigue and general malaise.
Interleukin-6 (IL-6) & Its Role in Pain
Interleukin-6 is another key pro-inflammatory cytokine strongly implicated in chronic prostatitis. It’s produced by a wide range of cells, including prostate epithelial cells, immune cells, and fibroblasts. IL-6 plays a critical role in the acute phase response but prolonged elevation contributes to chronic inflammation and tissue remodeling within the prostate.
Importantly, IL-6 is also closely linked to pain pathways. It can sensitize nociceptors (pain receptors) leading to heightened pain perception, contributing to the often debilitating pelvic pain experienced by patients with CP/CPPS. Its role in both inflammation and pain makes it a crucial target for therapeutic interventions.
The Influence of Chemokines & Immune Cell Recruitment
While cytokines initiate and amplify the inflammatory response, chemokines act as attractants, guiding immune cells to the site of inflammation. In chronic prostatitis, several chemokines like CCL2 (monocyte chemoattractant protein-1) are upregulated, drawing monocytes and macrophages into the prostate gland. These recruited immune cells then further release pro-inflammatory cytokines, perpetuating the cycle.
The specific types of immune cells infiltrating the prostate also influence the disease process. For example, an increase in T helper 1 (Th1) cells – which promote cell-mediated immunity – has been observed in chronic prostatitis patients, contributing to ongoing tissue damage and inflammation. Understanding these complex interactions between cytokines, chemokines, and immune cell populations is vital for developing more effective treatments that modulate the inflammatory response.
The complexity of cytokine involvement in chronic prostatitis highlights the challenges in finding a single ‘cure’ for the condition. Current research focuses on strategies to dampen down the overall inflammatory response, target specific cytokines implicated in pain pathways, or restore balance between pro- and anti-inflammatory signals. Further investigations are necessary to fully elucidate the intricate interplay between these signaling molecules and identify personalized therapeutic approaches that address the underlying mechanisms driving chronic prostatitis symptoms. The future of treatment likely lies in a multi-faceted approach combining pharmacological interventions with lifestyle modifications and pelvic floor rehabilitation to effectively manage this debilitating condition.