The prostate gland, often discussed in relation to aging men, is susceptible to various conditions, one of which is prostatitis – inflammation of the prostate. While traditionally understood through infection or anatomical factors, emerging research reveals a more intricate connection between the gut microbiome and this common ailment. The inflammatory processes inherent in both gut dysbiosis (an imbalance in the gut bacteria) and chronic prostatitis can create a feedback loop, exacerbating symptoms and potentially hindering effective treatment. Understanding this link isn’t about replacing conventional medical approaches but rather recognizing an additional layer of complexity that could unlock more holistic and preventative strategies.
Chronic prostatitis is notoriously difficult to treat, with many men experiencing persistent pain, urinary issues, and reduced quality of life even after antibiotic courses or other interventions. This difficulty highlights the need to explore factors beyond traditional causes. The gut microbiome, acting as a key regulator of immune function and inflammation throughout the body, presents a compelling area of investigation. A compromised gut environment can lead to increased intestinal permeability – often called “leaky gut” – allowing bacterial products and inflammatory molecules to enter the bloodstream, potentially triggering systemic inflammation that impacts distant organs like the prostate. The interplay between these systems is now being recognized as crucial for understanding chronic conditions.
Gut Microbiome & Inflammation: A Systemic Connection
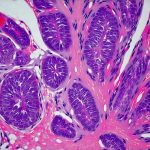
The human gut harbors trillions of microorganisms, collectively known as the microbiome. This complex ecosystem plays a pivotal role in digestion, nutrient absorption, immune system development, and even mental health. Dysbiosis, an imbalance within this microbial community – often characterized by a reduction in beneficial bacteria and an overgrowth of potentially harmful ones – can disrupt these functions, leading to chronic inflammation. This isn’t simply localized to the gut; it’s a systemic issue. Inflammatory molecules released from a dysbiotic gut can travel throughout the body via the bloodstream, impacting various organs and tissues.
The connection between gut health and systemic inflammation is mediated by several mechanisms. For instance, lipopolysaccharide (LPS), a component of Gram-negative bacteria commonly found in the gut, can trigger an immune response when it enters the circulation due to increased intestinal permeability. This response activates inflammatory pathways like NF-κB, leading to the release of pro-inflammatory cytokines – signaling molecules that amplify inflammation throughout the body. Furthermore, dysbiosis can impair the production of short-chain fatty acids (SCFAs), beneficial metabolites produced by gut bacteria during fiber fermentation. SCFAs have anti-inflammatory properties and contribute to gut barrier integrity, so a deficiency can exacerbate inflammatory processes.
This systemic inflammation creates an environment where chronic conditions like prostatitis can develop or worsen. The prostate gland is particularly vulnerable because of its proximity to the rectum and the potential for bacterial translocation from the gut. Furthermore, the immune system, constantly stimulated by gut-derived inflammatory signals, may become dysregulated, leading to inappropriate responses that contribute to prostatic inflammation. Understanding the link between blood sugar levels and inflammation is crucial in this context.
Prostatitis & Gut Dysbiosis: A Potential Bi-Directional Relationship
The relationship between prostatitis and gut dysbiosis appears to be bi-directional – meaning each can influence the other. Chronic inflammation associated with prostatitis can itself disrupt the gut microbiome, creating a vicious cycle. For example, prolonged use of antibiotics, often prescribed for suspected bacterial prostatitis (even if ultimately ineffective in chronic cases), can significantly alter the composition of the gut microbiota, reducing microbial diversity and promoting dysbiosis. Stress, commonly experienced by individuals living with chronic pain conditions like prostatitis, is another factor that can negatively impact gut health.
Conversely, a pre-existing state of gut dysbiosis may increase susceptibility to developing prostatitis or experiencing more severe symptoms. Studies are beginning to show differences in the gut microbiome composition of men with and without chronic prostatitis/chronic pelvic pain syndrome (CPPS). Specifically, some research suggests lower levels of beneficial bacteria like Lactobacillus and Bifidobacterium, coupled with higher levels of potentially pathogenic bacteria, in individuals with CPPS. This imbalance can contribute to increased intestinal permeability, systemic inflammation, and a compromised immune system – all factors that could play a role in the development or exacerbation of prostatitis symptoms. The precise nature of these microbial shifts and their causal relationship with prostatitis are still being investigated, but the emerging evidence is compelling.
Exploring Potential Mechanisms
The link between gut dysbiosis and prostatitis isn’t simply about inflammation; it’s also about immune modulation. The gut microbiome profoundly influences the development and function of the immune system. A healthy gut promotes a balanced immune response, while dysbiosis can lead to immune dysregulation, contributing to chronic inflammation and autoimmune reactions. In the context of prostatitis, this could mean an overactive or misdirected immune response targeting the prostate gland, even in the absence of infection.
- Immune Cell Trafficking: Gut dysbiosis can influence the trafficking of immune cells throughout the body. For instance, altered gut permeability allows for increased migration of leukocytes – white blood cells involved in inflammation – to distant sites like the prostate.
- Cytokine Production: The gut microbiome influences the production of cytokines, signaling molecules that regulate immune responses. Dysbiosis can lead to an imbalance in cytokine profiles, favoring pro-inflammatory pathways and contributing to chronic prostatic inflammation.
- Microbial Metabolites: As mentioned earlier, microbial metabolites like SCFAs play a vital role in regulating immune function. A deficiency in SCFA production due to dysbiosis can impair immune cell activity and exacerbate inflammatory processes.
Another crucial aspect is the potential for microbiome-mediated prostate infection. Although often considered non-bacterial, chronic prostatitis may involve low-grade infections that are difficult to detect with conventional methods. The gut microbiome can influence the susceptibility to these infections by modulating the local immune environment and potentially contributing to biofilm formation – a protective layer around bacteria that makes them resistant to antibiotics. Understanding the link between gut inflammation and prostatitis is vital for treatment.
Dietary Interventions & Probiotic Support
While more research is needed, dietary interventions aimed at restoring gut health offer promising avenues for managing prostatitis symptoms. A diet rich in fiber from fruits, vegetables, and whole grains promotes the growth of beneficial gut bacteria and increases SCFA production. Reducing processed foods, sugar, and unhealthy fats can help minimize inflammation and support a healthier microbiome. Fermented foods, such as yogurt, kefir, sauerkraut, and kimchi, are natural sources of probiotics – live microorganisms that can contribute to microbial diversity.
However, it’s important to note that probiotics aren’t one-size-fits-all. Different strains have different effects, and the optimal probiotic for an individual with prostatitis may vary depending on their specific gut microbiome composition and symptom profile. Consulting a healthcare professional or registered dietitian specializing in gut health can help identify appropriate probiotic supplements.
Future Research & Personalized Approaches
The emerging understanding of the gut-prostate connection opens doors to more personalized approaches to prostatitis management. Analyzing the gut microbiome through stool testing could provide valuable insights into an individual’s microbial profile, guiding dietary and lifestyle interventions tailored to their specific needs. Further research is needed to identify specific microbial signatures associated with different subtypes of prostatitis and to determine the optimal probiotic strains for restoring gut health and alleviating symptoms. Understanding the link between food additives and pelvic pain can also play a role in preventative care.
Ultimately, addressing gut dysbiosis may not be a cure-all for prostatitis, but it represents an important adjunctive therapy that could complement conventional treatments and improve long-term outcomes. Recognizing the intricate interplay between the gut microbiome, immune system, and prostate gland is crucial for developing more holistic and effective strategies for managing this challenging condition. It’s also worth exploring how kidney stones can affect overall health.