Prostatitis, inflammation of the prostate gland, is a surprisingly common condition affecting men of all ages, though more frequently those over 50. It manifests in various forms, from acute bacterial infections requiring immediate treatment to chronic conditions characterized by persistent pain and discomfort. While often localized as a urological issue, emerging research increasingly points towards a complex interplay between the gut microbiome, systemic inflammation, and prostate health. Understanding this connection is crucial for a more holistic approach to managing prostatitis and improving patient outcomes.
The traditional view of prostatitis focused heavily on bacterial infections or anatomical factors within the pelvic region. However, recent scientific investigations have begun to reveal a far more intricate picture where gut dysbiosis – an imbalance in the composition of gut bacteria – can contribute significantly to chronic inflammation throughout the body, potentially exacerbating or even initiating prostatic inflammation. This article will explore the growing evidence linking gut health and prostatitis, outlining potential mechanisms and future directions for research.
The Gut-Prostate Axis: A Developing Understanding
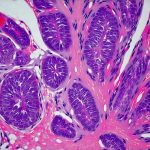
The connection between the gut and distant organs like the prostate isn’t as far-fetched as it might seem. It’s built upon the concept of the “gut-brain axis”, now expanding to include other organ systems, recognizing that a healthy gut microbiome is fundamental for overall health and immune regulation. The gut contains trillions of microorganisms, collectively known as the gut microbiota, which play vital roles in digestion, nutrient absorption, and crucially, immune system development and modulation.
An imbalanced gut microbiome can lead to increased intestinal permeability – often referred to as “leaky gut” – allowing bacterial products and toxins to enter the bloodstream, triggering systemic inflammation and potentially affecting organs far removed from the digestive tract, including the prostate gland. The relationship is bidirectional; prostate inflammation can also influence gut health, creating a cycle of chronic inflammation.
Exploring the Mechanisms
Inflammatory Pathways & Systemic Inflammation
Chronic prostatitis, particularly the non-bacterial forms (chronic prostatitis/chronic pelvic pain syndrome – CP/CPPS), often involves persistent low-grade systemic inflammation. The gut microbiome plays a major role in modulating inflammatory responses. Dysbiosis can lead to an overgrowth of pro-inflammatory bacteria and a reduction in those that produce anti-inflammatory compounds, like short-chain fatty acids (SCFAs). SCFAs, such as butyrate, are produced by beneficial bacteria during the fermentation of dietary fiber and have been shown to strengthen the gut barrier, reduce inflammation, and even impact immune cell function.
Reduced SCFA production coupled with increased levels of lipopolysaccharide (LPS), a toxin released from Gram-negative bacteria in the gut when permeability is compromised, contributes to systemic inflammatory processes that can affect prostate health. Elevated levels of pro-inflammatory cytokines like TNF-alpha and IL-6 have been found in both prostatitis patients and those with significant gut dysbiosis, further highlighting this connection.
The Role of Immune Dysregulation
The immune system is central to the development and progression of prostatitis. A healthy gut microbiome is essential for proper immune cell development and function. Approximately 70-80% of the body’s immune cells reside in the gut, making it a key training ground for the immune system. Gut dysbiosis can disrupt this delicate balance, leading to immune dysregulation and an increased risk of autoimmune reactions or chronic inflammation.
In prostatitis, this may manifest as inappropriate activation of the immune system within the prostate gland, contributing to pain and discomfort even in the absence of bacterial infection. Furthermore, alterations in gut bacteria can impact T-cell populations and cytokine production, influencing the body’s ability to effectively respond to infections and resolve inflammation within the prostate.
Dietary Influences & Microbiome Modulation
Diet plays a significant role in shaping the composition of the gut microbiome. A diet high in processed foods, sugar, and saturated fats can promote the growth of harmful bacteria and contribute to dysbiosis, while a diet rich in fiber, fruits, vegetables, and fermented foods supports a diverse and balanced microbiome. Specific dietary patterns have been linked to both increased and decreased risk of prostatitis symptoms.
For example, diets lacking adequate fiber can reduce SCFA production, weakening the gut barrier and increasing inflammation. Conversely, incorporating probiotic-rich foods or supplements – containing live beneficial bacteria – may help restore microbial balance and improve immune function. However, it’s important to note that probiotics are not a one-size-fits-all solution, and individual responses can vary significantly. Personalized dietary approaches tailored to specific microbiome profiles may be the most effective strategy for managing gut health and potentially mitigating prostatitis symptoms.
Ultimately, the research linking gut inflammation and prostatitis is still evolving, but the evidence strongly suggests a significant connection. Addressing gut health through dietary modifications, lifestyle changes, and perhaps targeted interventions like probiotics or prebiotics (foods that feed beneficial bacteria) may offer a valuable adjunct to traditional treatments for prostatitis and contribute to improved long-term outcomes. Future research will focus on identifying specific microbial signatures associated with different types of prostatitis, developing personalized microbiome-based therapies, and further elucidating the complex interplay between gut health, inflammation, and prostate function. It is crucial to consult healthcare professionals for accurate diagnosis and appropriate treatment plans tailored to individual needs.