Epithelial cells are arguably one of the most fundamental building blocks of the human body. They form protective barriers – like skin – and linings throughout our organs, including the digestive tract, lungs, kidneys, and even blood vessels. These cells aren’t just static walls though; they’re incredibly dynamic, constantly renewing themselves and playing crucial roles in secretion, absorption, protection, and sensory reception. Because of their pervasive nature and essential functions, understanding what constitutes “normal” epithelial cell counts is vital for assessing overall health and diagnosing a wide range of conditions. However, defining “normal” isn’t always straightforward, as it varies significantly based on location within the body, age, and even individual factors.
The challenge arises because epithelial cells are everywhere. Their natural shedding and renewal process means they’re frequently found in bodily fluids like urine, sputum, and even blood – albeit usually in small numbers. Determining when these counts indicate a healthy state versus a potential issue requires careful consideration of the specific context. A slightly elevated count in one area might be perfectly normal, while the same number in another could signal inflammation or disease. This article will explore what constitutes typical epithelial cell ranges, focusing on commonly tested areas and providing insights into interpreting results. It’s important to note that this information is for general understanding only and should not be used as a substitute for professional medical advice.
Understanding Epithelial Cell Counts in Common Bodily Fluids
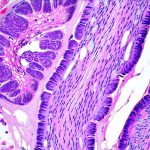
Epithelial cells are routinely assessed in various clinical tests, most notably urine analysis and sputum cytology. In urine, the presence of epithelial cells isn’t necessarily alarming; healthy individuals typically have a small number due to the natural shedding from the urinary tract. However, increased counts can indicate inflammation, infection (like a urinary tract infection – UTI), kidney disease, or even certain types of cancer. The type of epithelial cell present is also important – renal tubular epithelial cells suggest kidney damage, while urothelial cells are more common in bladder issues. In sputum, an analysis of mucus coughed up from the lungs, elevated counts can point to respiratory infections, inflammation (like asthma or COPD), or potentially lung cancer. Again, identifying the specific type of cell is critical for accurate diagnosis.
The “normal” range for epithelial cells varies based on the methodology used in the lab and the population being tested. Many labs report these cells as “few,” “moderate,” or “many,” rather than precise numerical counts. However, a general guideline for urine analysis would be: few (0-4 per high power field), moderate (5-20), and many (>20). Sputum cytology reports are often more qualitative, focusing on the presence of atypical cells that might suggest malignancy. It’s crucial to remember that these numbers serve as a starting point for further investigation; they aren’t definitive diagnoses in themselves. A physician will consider epithelial cell counts alongside other clinical findings and test results to form a complete picture.
The interpretation isn’t always simple, even with specific numbers. For example, dehydration can artificially inflate epithelial cell counts in urine because it concentrates the sample. Similarly, vigorous exercise or menstruation can also temporarily increase cell shedding. Therefore, healthcare professionals must consider the patient’s overall health status and potential contributing factors when interpreting these results. Context is everything when assessing epithelial cell counts—a seemingly high number might be entirely benign in one situation, while requiring further investigation in another. Understanding what constitutes a normal range can also be clarified by reviewing a normal specific gravity range in urine.
Factors Influencing Epithelial Cell Counts
Numerous factors can influence the quantity of epithelial cells found in bodily fluids, beyond just hydration and exercise. Age plays a role; older adults generally have more cellular debris shedding due to natural tissue aging and decreased organ function. Certain medical conditions like diabetes or autoimmune diseases can also increase inflammation, leading to higher counts. Moreover, medications – particularly those affecting kidney function or immune response – might alter cell shedding rates.
- Lifestyle factors such as smoking and diet can also contribute to changes in epithelial cell populations.
- Exposure to environmental toxins or irritants may cause increased cellular turnover and shedding.
- Catheter use or other invasive procedures can introduce inflammation and potentially elevate cell counts.
It’s essential for healthcare providers to obtain a thorough patient history, including all relevant medical conditions, medications, lifestyle habits, and recent procedures, when evaluating epithelial cell results. This holistic approach ensures more accurate interpretation and minimizes the risk of misdiagnosis. The lab methodology employed also matters; different techniques can yield slightly varying results, so it’s important for labs to adhere to standardized protocols.
Cell Type Identification: Beyond Just Counting
Simply counting epithelial cells is often insufficient. Identifying which type of epithelial cell is present provides significantly more diagnostic value. Different types indicate different sources and potential problems. For example, squamous epithelial cells are typically found in the upper urinary tract and their presence in a urine sample can suggest contamination from the skin around the collection site. Transitional epithelial cells originate from the bladder and ureters; their increased number may signal inflammation or even cancer within those structures. Renal tubular epithelial cells signify damage to the kidneys themselves.
Similarly, in sputum samples, identifying squamous cells versus columnar cells – which come from deeper respiratory passages – helps determine the severity of a lung condition. The presence of atypical squamous cells is often a red flag for potential malignancy. Advanced techniques like flow cytometry and immunohistochemistry can be used to further characterize epithelial cell types and identify specific markers associated with disease. Accurate identification of cell type is paramount for making informed clinical decisions, which may require various imaging scans for diagnosis.
Interpreting Results & Next Steps
When epithelial cell counts are elevated, the next steps depend on the context and other findings. A physician will typically order additional tests to investigate the underlying cause. For urine analysis, this might include a urine culture to identify any bacterial infection, or blood tests to assess kidney function. In sputum cytology, further imaging studies like a chest X-ray or CT scan may be necessary to evaluate for lung lesions or other abnormalities.
- It’s vital to avoid self-diagnosis and instead rely on the expertise of a healthcare professional.
- Follow-up testing might involve more specialized investigations, such as cystoscopy (for bladder issues) or bronchoscopy (for lung problems).
- Treatment will vary depending on the underlying cause, ranging from antibiotics for infections to surgery or chemotherapy for cancer.
Remember that epithelial cell counts are just one piece of the puzzle. They provide valuable information but must be interpreted within the broader clinical picture. A collaborative approach between patients and healthcare providers is essential to ensure accurate diagnosis and appropriate management. The goal isn’t simply to lower cell counts, but to address the underlying cause of their elevation and restore overall health. If cancer is a concern, understanding the chances of cancer returning can be an important part of the process.