Bladder dysfunction impacts millions worldwide, significantly reducing quality of life. Traditional treatments often focus on behavioral therapies, medications aimed at muscle relaxation, or surgical interventions addressing structural issues. However, the intricate relationship between nerves and bladder function is increasingly recognized, leading to a growing interest in nerve-targeting drugs as a novel therapeutic approach. These aren’t simply about suppressing symptoms; they aim to modulate the nervous system’s influence on the bladder, offering potentially more targeted and enduring relief for conditions like overactive bladder (OAB), interstitial cystitis/bladder pain syndrome (IC/BPS), and neurogenic bladder. Understanding this evolving field requires delving into the specifics of how these drugs work, what conditions they address, and where future research is headed.
The nervous system plays a critical role in every aspect of bladder control – from filling and storage to emptying. Signals travel along complex pathways between the brain, spinal cord, and the bladder itself. Disruptions within these pathways can manifest as various bladder dysfunctions. Nerve-targeting drugs seek to re-establish proper neurological control, either by blocking pain signals, modulating nerve impulses, or even promoting nerve regeneration in some cases. This is a departure from traditional therapies that often address only the symptoms of bladder dysfunction without tackling the underlying neurological causes. It’s important to note that this field is still developing, and many nerve-targeting approaches are currently under investigation or used off-label, meaning they have not yet received widespread regulatory approval for specific bladder conditions.
The Science Behind Nerve Targeting
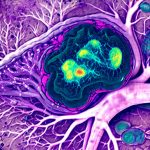
Nerve targeting in bladder therapy isn’t a single technique but encompasses various strategies aimed at influencing the nervous system’s role in bladder function. At its core is understanding neuropathic pain – chronic pain caused by damage or disease affecting the nervous system. Many bladder conditions, particularly IC/BPS, involve significant neuropathic components. Drugs designed to block specific nerve receptors or channels can interrupt these pain signals. For example, medications targeting P2X3 receptors, found on sensory nerves in the bladder, are showing promise in reducing bladder pain and urgency. Another approach focuses on modulating the autonomic nervous system, which controls involuntary functions like bladder emptying. This involves drugs that influence neurotransmitters like acetylcholine, impacting bladder contractility and storage capacity.
The key difference between nerve-targeting drugs and traditional pharmacological approaches lies in their selectivity. Traditional medications often have broader effects, potentially leading to side effects. Nerve-targeting aims for greater precision, minimizing off-target impacts. This selectivity is achieved through several mechanisms: targeted drug delivery systems (like intravesical injections), the use of antibodies that specifically bind to nerve receptors, or even gene therapy approaches aimed at modifying nerve function. It’s also crucial to appreciate the concept of neuroplasticity – the brain’s ability to reorganize itself by forming new neural connections throughout life. Some nerve-targeting strategies aim to harness this plasticity, promoting beneficial changes in nerve pathways over time.
Ultimately, successful nerve targeting relies on a deep understanding of the specific neurological mechanisms underlying each bladder condition and tailoring treatment accordingly. This requires advanced diagnostic tools to identify which nerves are malfunctioning and personalize therapy for individual patients. The goal isn’t simply to suppress symptoms but to restore healthy neural control of the bladder, leading to long-term improvement in function and quality of life.
Current Applications & Emerging Therapies
Currently, nerve-targeting drugs are primarily used off-label or in clinical trials for conditions where traditional treatments have proven inadequate. One notable example is onabotulinumtoxinA (Botox), originally approved for cosmetic purposes, but now frequently used intravesically to treat refractory OAB. Botox works by temporarily paralyzing the detrusor muscle (the bladder’s main contracting muscle) via inhibition of acetylcholine release from nerve endings, reducing involuntary contractions and urgency. While effective, its effects are temporary, requiring repeated injections every 6-9 months.
Beyond Botox, several other nerve-targeting therapies are in development or showing promise: – P2X3 receptor antagonists for IC/BPS – these drugs aim to reduce bladder pain by blocking sensory nerves. – Nerve growth factor (NGF) inhibitors – NGF plays a role in neuropathic pain; inhibiting it may alleviate chronic bladder pain. – Spinal cord stimulation – implantable devices that deliver electrical pulses to modulate nerve signals, showing promise for neurogenic bladder and IC/BPS. – Gene therapy approaches – still experimental, these aim to modify nerve function directly within the bladder wall. The future of bladder therapy is leaning towards a more personalized approach utilizing biomarkers to identify patients who will benefit from specific nerve-targeting interventions.
Targeting Sensory Nerves for Pain Relief
Chronic bladder pain, as seen in IC/BPS, is often driven by heightened sensitivity and abnormal signaling in sensory nerves within the bladder wall. These nerves express various receptors that contribute to pain perception. P2X3 receptors are a prime target because they play a crucial role in transmitting pain signals from the bladder to the brain. Several pharmaceutical companies are developing highly selective P2X3 antagonists, aiming to block these receptors and reduce bladder pain without significantly impacting other bodily functions. Clinical trials have shown some promising results, with patients experiencing reduced pain levels and improved quality of life.
However, challenges remain in developing effective P2X3 antagonists. One key issue is receptor desensitization – prolonged blockade can lead to the receptor becoming less responsive over time, reducing drug efficacy. Another challenge is ensuring sufficient drug penetration into the bladder wall to reach the target nerves effectively. Researchers are exploring various strategies to overcome these hurdles, including developing novel drug formulations and delivery methods. The ideal scenario would involve a long-lasting, highly selective P2X3 antagonist that provides sustained pain relief with minimal side effects.
Furthermore, understanding the complex interplay between different sensory nerve receptors is crucial. Targeting only one receptor may not be sufficient for complete pain control; combination therapies targeting multiple receptors could offer more comprehensive relief. Future research will focus on identifying these synergistic targets and developing personalized treatment strategies based on individual patient profiles.
Modulating Autonomic Nervous System Control
The autonomic nervous system regulates involuntary functions, including bladder storage and emptying. Disruptions in this system can lead to OAB, neurogenic bladder, or urinary retention. Nerve-targeting drugs can modulate the autonomic nervous system by influencing neurotransmitter levels or directly affecting nerve pathways. For instance, medications like anticholinergics reduce bladder contractility by blocking acetylcholine receptors, decreasing urgency and frequency. However, these have broad effects causing side effects like dry mouth and constipation.
More targeted approaches involve selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs). While primarily known as antidepressants, these medications can also influence bladder function by modulating neurotransmitter levels in the spinal cord and brain, affecting bladder storage capacity and contractility. These are often used off-label for OAB when first-line treatments fail. Another emerging strategy is to modulate peripheral autonomic nerves directly through techniques like percutaneous tibial nerve stimulation (PTNS), which stimulates a nerve in the ankle to influence bladder control.
The challenge lies in achieving a balance between reducing unwanted contractions and preserving healthy bladder function. Overly suppressing autonomic activity can lead to urinary retention or incomplete emptying. Personalized treatment plans, guided by individual patient characteristics and response to therapy, are essential for optimizing outcomes. Future research will focus on identifying biomarkers that predict responsiveness to specific autonomic modulation therapies.
Exploring Neuroregenerative Approaches
The most ambitious – and currently experimental – nerve-targeting strategies involve promoting nerve regeneration within the bladder wall. Damage or injury to nerves can disrupt bladder function, leading to chronic pain or incontinence. Nerve growth factor (NGF) plays a crucial role in neuronal survival and growth. Delivering NGF directly to the bladder, either through injections or gene therapy, could potentially stimulate nerve repair and restore lost neurological control.
However, NGF delivery is complex. Systemic administration can cause significant side effects. Researchers are exploring localized delivery methods using biocompatible scaffolds or viral vectors to target NGF specifically to damaged nerves within the bladder wall. Gene therapy approaches aim to introduce genes encoding for NGF or other neurotrophic factors directly into bladder tissues, promoting long-term nerve regeneration.
These regenerative strategies remain in early stages of development but hold immense promise for treating chronic bladder dysfunction caused by nerve damage. The key challenges include ensuring efficient gene delivery, minimizing immune responses, and demonstrating sustained nerve regeneration and functional improvement. While still years away from widespread clinical application, neuroregenerative approaches represent a paradigm shift in bladder therapy – moving beyond symptom management to restore the underlying neurological causes of dysfunction.