Mast cells are pivotal players in the body’s immune response, often recognized for their role in allergic reactions. However, their influence extends far beyond these immediate hypersensitivity events, impacting a wide range of physiological processes including wound healing and tissue remodeling. These resident immune cells reside strategically within tissues, acting as sentinels that detect harmful stimuli – from pathogens to damaged cells – and initiating an inflammatory cascade to restore homeostasis. Understanding the nuanced function of mast cells is crucial, especially when considering chronic inflammatory conditions like those affecting the bladder, where their contribution can be both protective and detrimental depending on the context and stage of disease.
Bladder inflammation, encompassing conditions such as interstitial cystitis/bladder pain syndrome (IC/BPS) and overactive bladder (OAB), presents a significant clinical challenge due to its complex etiology and often elusive pathophysiology. While historically thought to be largely idiopathic, growing evidence points to immune dysregulation as a central feature of these disorders. Mast cells are increasingly recognized as key contributors to this dysregulation, releasing a plethora of inflammatory mediators that can exacerbate bladder symptoms like pain, urgency, and frequency. Investigating the specific roles mast cells play in different stages of bladder inflammation is paramount for developing targeted therapies that address the underlying causes of these debilitating conditions – rather than simply managing their symptoms. It’s also important to consider related areas of urology such as kegels and how they can impact bladder health.
Mast Cell Activation and Inflammatory Mediators
Mast cell activation occurs through a variety of stimuli including direct pathogen recognition, IgE-mediated responses to allergens, or even physical/chemical irritants. Once activated, mast cells undergo degranulation, releasing preformed mediators such as histamine, tryptase, and chymase. These immediate effects are often responsible for the acute symptoms associated with allergic reactions but also contribute significantly to inflammatory processes in chronic conditions. Beyond degranulation, mast cells synthesize de novo lipid mediators like prostaglandins and leukotrienes, along with cytokines and growth factors that modulate immune cell recruitment and tissue remodeling.
The complexity of mast cell activation is further compounded by the fact they can be activated via different receptors leading to distinct outcomes. For example, stimulation through Toll-like receptors (TLRs) elicits a pro-inflammatory response, while activation of adenosine receptors can have immunosuppressive effects. This plasticity highlights the dynamic nature of mast cells and their capacity to both promote and resolve inflammation depending on the specific signals they receive within the bladder microenvironment. Moreover, recent research suggests that mast cell mediators aren’t just passively released but actively shape the bladder environment by influencing urothelial cell function and neuronal sensitivity – contributing directly to pain perception.
The role of these mediators in bladder inflammation is multifaceted. Histamine increases vascular permeability leading to edema and potentially exacerbating urgency. Tryptase, a serine protease, can activate other inflammatory cells and contribute to tissue damage. Leukotrienes are potent chemoattractants for neutrophils and eosinophils further amplifying the inflammatory cascade. Cytokines like TNF-α and IL-6 recruit more immune cells and promote chronic inflammation while growth factors contribute to fibrosis and structural changes within the bladder wall. Understanding which mediators dominate at different stages of bladder disease is essential for developing targeted therapeutic strategies. In some cases, understanding diuretics may be helpful as well.
Mast Cells in Bladder Disease Pathogenesis
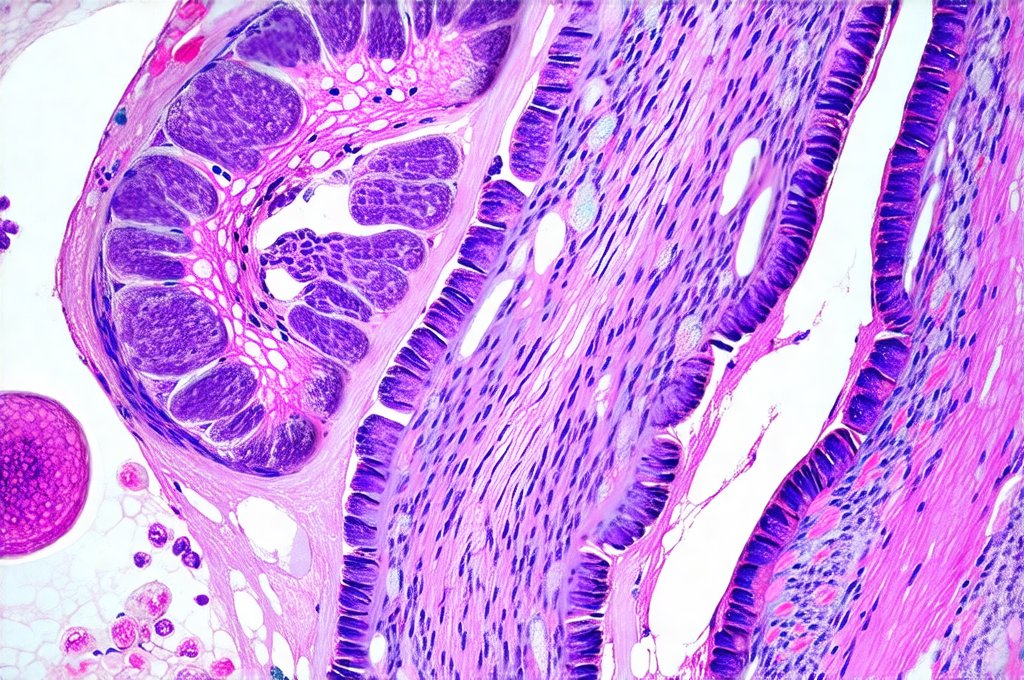
In IC/BPS, mast cell numbers are often elevated within the bladder wall, particularly in areas of inflammation. This increase is frequently accompanied by evidence of mast cell activation – demonstrable through increased levels of histamine metabolites and tryptase in urine or bladder biopsies. Several theories attempt to explain this heightened mast cell presence and activity. One prevailing hypothesis suggests that a defect in the bladder epithelium allows for increased permeability to antigens, triggering an IgE-mediated immune response and subsequent mast cell activation. Another proposes that chronic irritation from acidic urine or other factors leads to direct mast cell stimulation.
However, it’s becoming increasingly clear that mast cells aren’t merely reactive bystanders but actively contribute to the perpetuation of bladder inflammation. They release mediators that damage urothelial cells compromising their barrier function and creating a vicious cycle of inflammation. Furthermore, mast cell activation can sensitize nociceptors (pain receptors) in the bladder wall – lowering the threshold for pain perception and contributing to chronic pelvic pain. In OAB, while mast cell density isn’t always as dramatically increased as in IC/BPS, their influence on detrusor muscle hyperactivity is significant; mediators released by activated mast cells can directly affect smooth muscle contractility and contribute to unstable bladder function.
The interplay between mast cells and other immune cells within the bladder microenvironment is also crucial. Activated mast cells release chemokines that recruit neutrophils, macrophages, and T cells further amplifying inflammation. They can also influence T cell differentiation promoting Th2 responses which are often observed in IC/BPS patients. This complex immunologic network underscores the need for a holistic approach to understanding and treating bladder disease – targeting multiple immune pathways rather than focusing solely on mast cells themselves. If biopsy is needed, it’s important to understand its role in diagnosis as well.
The Role of Mast Cell-Urothelium Interactions
The urothelium, the specialized lining of the bladder, isn’t simply a passive barrier but actively participates in immune regulation. In healthy bladders, the urothelium produces factors that suppress inflammation and maintain immune homeostasis. However, in inflamed bladders this function is often impaired, leading to increased permeability and activation of underlying immune cells including mast cells. Mast cell mediators like tryptase can further damage the urothelium exacerbating barrier dysfunction and creating a positive feedback loop of inflammation.
Recent studies have demonstrated that activated mast cells release factors that alter urothelial cell gene expression – promoting the production of pro-inflammatory cytokines and chemokines. This creates a microenvironment that sustains chronic inflammation and contributes to bladder wall remodeling. Furthermore, mast cell mediators can directly affect urothelial permeability increasing the passage of antigens and triggering further immune activation. Restoring urothelial barrier function is therefore seen as a potential therapeutic target for mitigating bladder inflammation – alongside strategies aimed at modulating mast cell activity.
The interplay between mast cells and urothelial cells isn’t unidirectional; urothelial cells also influence mast cell behavior. For example, damaged or stressed urothelial cells release alarm signals like ATP that activate mast cells through purinergic receptors further amplifying the inflammatory response. This complex bidirectional communication highlights the need for a nuanced understanding of these interactions – as interventions targeting one component may inadvertently affect the other.
Mast Cells and Bladder Pain Mechanisms
Chronic pelvic pain is a hallmark symptom of IC/BPS and significantly impacts patients’ quality of life. While the precise mechanisms underlying bladder pain are still being elucidated, mast cells play a critical role in its development and maintenance. Activated mast cells release mediators that directly sensitize nociceptors – lowering the threshold for pain perception and contributing to hyperalgesia (increased sensitivity to pain). Histamine, substance P, and nerve growth factor (NGF) are key players in this process.
Furthermore, mast cell activation can lead to neuroinflammation – inflammation of the nerves themselves – which further exacerbates pain signaling. Mast cell mediators induce glial cell activation within the dorsal root ganglia – amplifying nociceptive transmission to the brain. This creates a chronic pain state that is difficult to treat with conventional analgesics. Recent research suggests that targeting mast cells or their mediators can effectively reduce bladder pain in pre-clinical models – offering promising avenues for therapeutic intervention.
Importantly, pain perception is subjective and influenced by psychological factors. Mast cell activation may contribute to central sensitization – a phenomenon where the brain becomes more sensitive to pain signals over time. This highlights the importance of multidisciplinary approaches to managing chronic bladder pain – incorporating not only pharmacological interventions but also psychological support and behavioral therapies.
Therapeutic Strategies Targeting Mast Cells
Given their central role in bladder inflammation, mast cells represent attractive therapeutic targets for IC/BPS and OAB. Several strategies are currently being investigated or have shown promise in preclinical studies. Antihistamines can block histamine receptors reducing some of the acute symptoms associated with mast cell activation but often fail to address the underlying chronic inflammatory process. Mast cell stabilizers like cromolyn sodium prevent degranulation – reducing the release of inflammatory mediators but may have limited efficacy in established inflammation.
More targeted approaches focus on inhibiting specific mast cell signaling pathways or depleting mast cells altogether. Blocking TLRs can reduce mast cell activation induced by bacterial products or other stimuli. Inhibiting histamine synthesis or leukotriene production can also modulate mast cell function and reduce inflammation. Emerging therapies include monoclonal antibodies targeting mast cell-specific receptors or cytokines – offering the potential for highly selective therapeutic effects.
However, it’s crucial to remember that completely eliminating mast cells may not be desirable as they play essential roles in tissue homeostasis and immune defense. The goal is to modulate their activity – restoring a balance between pro-inflammatory and anti-inflammatory responses – rather than eradicating them altogether. Future research will focus on identifying biomarkers that predict which patients are most likely to benefit from specific mast cell targeted therapies and developing personalized treatment strategies based on individual inflammatory profiles.