Interstitial Cystitis (IC), also known as Bladder Pain Syndrome (BPS), is a chronic condition causing bladder pain and urinary frequency/urgency. While its precise cause remains elusive, IC is believed to stem from a complex interplay of factors, rather than a single identifiable trigger. Current research points towards potential issues with the protective layer lining the bladder – called the urothelium – along with immune system dysfunction, nerve damage, and even psychological components contributing to symptom development. For many years, treatment options have been limited, focusing primarily on managing symptoms without addressing underlying pathology. However, growing evidence suggests that altered permeability of the bladder wall plays a significant role in initiating and perpetuating IC symptoms, opening up new avenues for understanding and potential therapeutic interventions.
Traditional thinking often focused on microscopic defects or ‘leaks’ within the urothelium as the primary source of irritation. But increasingly, it’s recognized that the permeability – how easily substances can pass through the bladder wall – is a key factor. A healthy bladder wall acts as a selective barrier, preventing potentially irritating substances present in urine from contacting underlying nerve endings and triggering inflammation. In IC, this barrier function appears compromised, allowing increased permeability. This allows for greater exposure of suburothelial nerves to components within the urine (like potassium ions, histamine, or even normal urinary metabolites), causing pain signals and initiating an inflammatory cascade that can perpetuate the cycle of bladder dysfunction. Understanding how and why this permeability changes is central to developing more effective treatments.
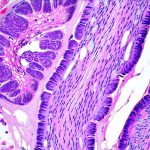
Bladder Wall Permeability & Urothelial Dysfunction
The urothelium isn’t simply a passive barrier; it’s a dynamic tissue actively regulating what passes through it. It achieves this through tight junctions – specialized protein structures that seal the spaces between bladder cells, preventing paracellular permeability (passage between cells). Additionally, transcellular transport mechanisms exist within the cells themselves, controlling substance movement through the cells. In IC bladders, studies have demonstrated alterations in both of these aspects. Specifically, research has shown a downregulation of key tight junction proteins like claudin-1 and occludin, essentially weakening the ‘seal’ between bladder cells. This leads to increased paracellular permeability. Furthermore, changes in aquaporin expression – water channel proteins – can also contribute to altered fluid balance within the bladder wall, impacting overall barrier function.
The reasons behind this urothelial dysfunction are multi-faceted. Chronic inflammation, often seen in IC patients, is a major contributor. Inflammatory mediators released by immune cells can directly damage tight junctions and disrupt cellular transport mechanisms. Another factor is oxidative stress – an imbalance between free radical production and antioxidant defense systems. Oxidative stress can also compromise urothelial integrity, leading to increased permeability. Finally, it’s believed that genetic predisposition may play a role in some cases, influencing the vulnerability of the bladder wall to these damaging factors. – It’s important to note that the exact mechanisms are still being investigated and likely vary between individuals with IC.
This compromised barrier function creates a vicious cycle: increased permeability leads to nerve activation, triggering inflammation, which further damages the urothelium, increasing permeability even more. This explains why symptoms often persist or worsen over time if left unaddressed. – Addressing this core issue of bladder wall permeability is therefore critical for long-term symptom management and potential disease modification.
The Role of Mast Cells & Neuroinflammation
Mast cells are immune cells residing in the bladder wall that play a significant role in IC pathogenesis, particularly in relation to increased permeability. These cells release various mediators – including histamine, proteases, and growth factors – that can directly damage urothelial tight junctions and increase vascular permeability (leading to edema and inflammation). In IC bladders, mast cell density is often significantly elevated compared to healthy controls. The activation of these mast cells can be triggered by a variety of stimuli, including urinary components, nerve impulses, or even psychological stress. – This highlights the complex interplay between the immune system, nervous system, and bladder wall in IC.
Beyond mast cells, neuroinflammation – inflammation affecting nerves – is now recognized as a key feature of IC. Activated nerves release neuropeptides like substance P and nerve growth factor (NGF), which further sensitize pain pathways and contribute to mast cell activation, creating another feedback loop that perpetuates the inflammatory response. NGF also promotes increased bladder wall permeability by directly affecting urothelial cells. This neuroinflammation is often triggered by the initial increase in permeability, as exposure of suburothelial nerves to urinary components initiates a cascade of events leading to nerve sensitization and inflammation. – This understanding has led to research into therapies targeting neuroinflammation, such as NGF inhibitors, showing promising results in some patients.
Understanding Permeability Testing & Biomarkers
Currently, there isn’t a single definitive ‘permeability test’ routinely used in clinical practice for IC diagnosis. However, researchers are actively investigating methods to assess bladder wall permeability in vivo and ex vivo. One approach involves measuring urinary levels of certain biomarkers that indicate barrier dysfunction. For example, elevated levels of albumin or other proteins in the urine can suggest increased paracellular permeability. More sophisticated techniques include analyzing urine samples for specific tight junction protein fragments, indicating breakdown of the urothelial seal. – These biomarker studies are still evolving and require further validation before they become standard diagnostic tools.
Another area of research involves using cystoscopy with fluorescence microscopy to visualize the bladder wall in vivo. By administering fluorescent dyes that highlight areas of increased permeability, clinicians can potentially identify regions of barrier dysfunction during a cystoscopic examination. This approach offers the advantage of directly visualizing the urothelium and assessing its integrity in real-time. – However, this technique is still experimental and requires specialized equipment and expertise.
Finally, ex vivo studies utilize bladder biopsies to assess permeability using Ussing chambers – devices that allow researchers to measure ion flux across bladder tissue samples under controlled conditions. This provides a more detailed assessment of barrier function but is invasive and doesn’t necessarily reflect the situation within the intact bladder. – Despite these challenges, ongoing research into permeability testing offers hope for developing objective tools to diagnose IC and monitor treatment response. What role does biopsy play in diagnosis?
Therapeutic Strategies Targeting Permeability
Given the central role of bladder wall permeability in IC pathogenesis, several therapeutic strategies are being explored to address this issue directly. One promising approach involves restoring tight junction function through supplementation with specific nutrients or compounds. For example, some studies have shown that oral administration of hyaluronic acid (HA) can help strengthen tight junctions and reduce permeability. – HA is a naturally occurring substance found in the bladder wall, and supplementing it may help restore barrier integrity.
Another strategy focuses on reducing inflammation and oxidative stress within the bladder wall. This includes using antioxidants to neutralize free radicals and anti-inflammatory agents to dampen down the immune response. Pentosan polysulfate sodium (PPS), a commonly used IC medication, has been shown to have both anti-inflammatory and barrier protective effects. – However, PPS doesn’t work for everyone, and its mechanism of action is still being investigated.
Emerging therapies also target mast cell activation and neuroinflammation. For example, certain antihistamines can help reduce mast cell degranulation and decrease histamine release, while NGF inhibitors may help dampen down neuroinflammatory pain pathways. – These newer approaches are still under investigation but hold promise for providing more targeted and effective treatment options. Ultimately, a multi-faceted approach that combines strategies to restore barrier function, reduce inflammation, and address nerve sensitization is likely to be the most effective way to manage IC symptoms long-term. What role do bladder instillations play in treating chronic cystitis?
Future Directions & Research Needs
While significant progress has been made in understanding the role of bladder wall permeability in IC, much research remains to be done. A key area for future investigation is identifying the specific factors that trigger urothelial dysfunction and lead to increased permeability in different individuals with IC. This will require large-scale studies examining genetic predisposition, environmental exposures, and immune system characteristics. – Personalized medicine approaches may ultimately be necessary to tailor treatments based on individual patient profiles.
Further research is also needed to develop more reliable and non-invasive methods for assessing bladder wall permeability in vivo. Biomarker discovery and the refinement of cystoscopic imaging techniques are crucial steps in this process. Finally, clinical trials evaluating novel therapeutic strategies targeting permeability – such as tight junction modulators, anti-inflammatory agents, and neuroinflammation inhibitors – are essential to translate research findings into effective treatments for IC patients. – Continued investment in research is vital to unraveling the complexities of IC and improving the lives of those affected by this chronic and debilitating condition. What role does flow testing play in recurrent retention? What role do kegels play in urology for women?