Bladder infections, often referred to as cystitis, and yeast infections, primarily vaginal candidiasis, are both incredibly common conditions affecting women – and sometimes men. While seemingly disparate in their origins and locations, the overlapping symptoms frequently lead to misdiagnosis, causing unnecessary worry, delayed treatment, and potentially inappropriate medication use. The similarities aren’t accidental; they stem from shared nerve pathways and anatomical proximity, meaning that sensations originating in one area can easily be misinterpreted as coming from another. This confusion is further amplified by the fact that many over-the-counter remedies are available for both conditions, encouraging self-diagnosis which often proves inaccurate. Understanding why UTIs are often misdiagnosed can help avoid unnecessary stress and treatment delays.
The core issue lies in the presentation of symptoms. Both infections can cause discomfort and irritation in the pelvic region, including burning sensations, itching, urgency, and frequency – all hallmarks of both cystitis and yeast infections. A woman experiencing these symptoms might understandably assume it’s a familiar yeast infection if she’s had one before, reaching for an anti-fungal cream or suppository without exploring other possibilities. This can be particularly problematic as delaying treatment for a bladder infection can lead to more serious complications like kidney infections. Understanding the subtle differences, and recognizing when professional medical evaluation is necessary, are crucial steps in ensuring appropriate care and preventing escalation of symptoms.
Overlapping Symptoms: A Source of Confusion
The reason these two conditions are so often confused begins with their shared symptom profile. Consider the classic signs: – Burning sensation during urination (dysuria) – present in both bladder infections and sometimes, though less commonly, in severe yeast infections causing external vulvar irritation. – Frequent urge to urinate – a hallmark of cystitis but also experienced by women who are anxious or stressed about their vaginal health, potentially exacerbating the perceived need to go frequently. – Itching and discomfort around the urethra – common in both, though typically more pronounced and localized in yeast infections affecting the vulva. – Pelvic pain – vague enough to be attributed to either condition, making differentiation difficult without a thorough examination.
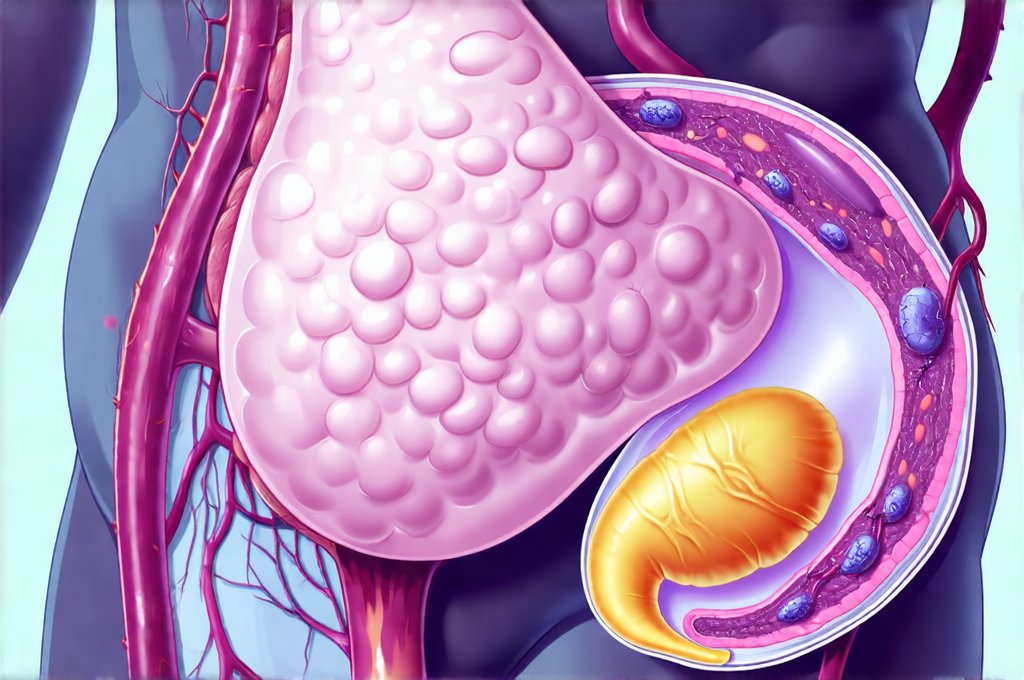
The anatomical proximity of the bladder and vagina plays a significant role. The urethra, through which urine passes, is located close to the vaginal opening. Inflammation or irritation in one area can easily radiate to the other, blurring the lines between symptoms. Moreover, the nervous system interprets signals from these areas similarly, contributing to misidentification of the source of discomfort. A woman might perceive a burning sensation originating from the bladder as coming from her vagina, leading her to believe she has a yeast infection when, in reality, it’s a urinary tract issue.
Finally, the common availability of over-the-counter treatments contributes to self-diagnosis and mismanaged care. Anti-fungal creams readily available for yeast infections offer quick relief for vulvar itching but do nothing for a bladder infection, potentially delaying appropriate antibiotic treatment. This highlights the importance of seeking professional medical advice before starting any course of treatment, even if it seems like a familiar condition.
Distinguishing Features: Clues to Accurate Diagnosis
While symptoms can overlap considerably, there are key differences that can help distinguish between a bladder infection and a yeast infection. A yeast infection typically presents with intense itching around the vulva and vagina, often accompanied by a thick, white, cottage cheese-like discharge. This discharge is usually odorless. Pain during sexual intercourse (dyspareunia) is also common. In contrast, a bladder infection primarily involves pain or burning during urination, frequent and urgent need to urinate, and potentially lower abdominal discomfort. The urine itself may appear cloudy or have a strong odor.
Looking at the nature of the discharge can be particularly helpful. While some women with bladder infections might experience increased vaginal discharge due to irritation, it won’t typically have the characteristic appearance of a yeast infection’s discharge. Similarly, if itching is the dominant symptom and burning during urination is minimal or absent, a yeast infection is more likely. However, these aren’t foolproof indicators, as some women with bladder infections can experience mild external irritation that mimics yeast infection symptoms.
It’s also important to consider other factors like recent antibiotic use. Antibiotics can disrupt the natural balance of bacteria in the vagina, increasing the risk of a yeast infection. If a woman has recently taken antibiotics and is experiencing vaginal itching, a yeast infection is more probable. Conversely, if there’s no history of antibiotic use and the primary symptom is burning during urination, a bladder infection should be strongly considered.
Recognizing Red Flags: When to See a Doctor
It’s vital to seek medical attention when symptoms are unclear or concerning. – Persistent Symptoms: If symptoms persist for more than a few days despite self-treatment, it’s crucial to see a doctor. This indicates the problem is unlikely to be a simple yeast infection and may require further investigation. – Fever or Chills: These are signs of a potentially serious complication like a kidney infection (pyelonephritis) resulting from an untreated bladder infection and necessitate immediate medical attention. – Back Pain: Flank pain, especially if accompanied by fever, is another indicator of a possible kidney infection. – Blood in Urine: This is never normal and requires prompt evaluation to rule out serious underlying conditions.
A healthcare provider can accurately diagnose the condition through simple tests. A urine analysis (urinalysis) can detect bacteria in the urine, confirming a bladder infection. A vaginal swab can identify the presence of yeast cells under a microscope, diagnosing a yeast infection. These tests are quick, painless and provide definitive answers, eliminating guesswork and ensuring appropriate treatment. It’s important to remember are all bladder infections considered UTIs?
Preventing Misdiagnosis: Proactive Steps
Preventing misdiagnosis starts with education and awareness. Understanding the differences between these two common conditions empowers women to make informed decisions about their health. – Avoid Self-Diagnosis: Resist the urge to self-treat based on past experiences or online information. A professional medical evaluation is always recommended, especially if symptoms are new or unusual. – Track Symptoms: Keeping a record of your symptoms – including when they started, what makes them better or worse, and any associated factors – can provide valuable information for your doctor. – Communicate Clearly: Be specific about your symptoms when describing them to your healthcare provider. Don’t hesitate to ask questions if you’re unsure about anything.
Long-Term Health & Recurrent Infections
Recurrent bladder infections or yeast infections can significantly impact a woman’s quality of life. If either condition recurs frequently, it’s essential to identify underlying causes and implement preventative measures. For bladder infections, this might involve lifestyle changes like staying well-hydrated, urinating after intercourse, and avoiding irritating substances like caffeine and alcohol. In some cases, prophylactic antibiotics or vaginal estrogen therapy may be recommended. For yeast infections, maintaining good hygiene practices, wearing breathable underwear, and avoiding douching can help prevent recurrence. Probiotic supplements containing lactobacilli strains have also shown promise in restoring the natural balance of vaginal flora. Understanding why some women get frequent bladder infections is a vital step toward prevention and effective management. Ultimately, a collaborative approach with your healthcare provider is key to managing these conditions effectively and minimizing their impact on your health and well-being.