Prostatitis, inflammation of the prostate gland, is a remarkably common condition affecting men of all ages, yet achieving full recovery can be surprisingly elusive. Often dismissed as simply an ‘old man’s problem,’ prostatitis manifests in diverse ways – from acute, debilitating pain to chronic discomfort that subtly impacts quality of life. The difficulty lies not just in diagnosing the specific type of prostatitis (acute bacterial, chronic bacterial, chronic prostatitis/chronic pelvic pain syndrome, and asymptomatic inflammatory prostatitis), but also in understanding the complex interplay between physiological factors, psychological stress, and lifestyle choices that contribute to its persistence. Many men experience prolonged symptoms even after initial treatment, leading to frustration, anxiety, and a sense of helplessness.
The reasons for this protracted recovery are multifaceted. Unlike infections with clear-cut cures, many forms of prostatitis don’t respond predictably to standard antibiotic treatments. Chronic inflammation can become self-perpetuating, involving complex immune responses and potentially altering the prostate’s own microenvironment. Furthermore, pelvic floor dysfunction – a tightening or weakness of the muscles supporting the bladder, bowel, and sexual organs – frequently accompanies prostatitis, exacerbating pain and creating a vicious cycle where muscle tension fuels further inflammation. Successfully navigating recovery demands a holistic approach that addresses not just the physical symptoms but also the emotional and lifestyle factors at play. It is important to understand when lower back pain can be an indicator of underlying issues.
Understanding the Challenges in Prostatitis Recovery
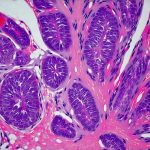
The prostate gland itself is deeply embedded within the pelvic region and intimately connected to other vital structures – the urethra, bladder neck, and seminal vesicles. This anatomical proximity means inflammation can easily spread or be influenced by conditions affecting neighboring organs. Moreover, the prostate’s role in urinary function and sexual health makes prostatitis symptoms particularly disruptive. The sheer variety of symptoms – pain in the groin, lower back, testicles, difficulty urinating, frequent urination, painful ejaculation – adds to the diagnostic challenge and complicates treatment selection. It’s not uncommon for men to undergo multiple tests and consultations before receiving a definitive diagnosis, contributing to delays in appropriate care.
A significant hurdle is that many cases of prostatitis are not caused by bacterial infection. Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS), the most common form, has an unknown etiology, meaning its root cause remains elusive. Theories abound, ranging from nerve damage and autoimmune responses to muscle imbalances and psychological factors, but a definitive explanation remains out of reach. This lack of clarity makes targeted treatment difficult; therapies are often aimed at managing symptoms rather than eradicating a specific underlying problem.
Finally, the prostate’s relatively poor blood supply can hinder medication delivery and slow down healing processes. Many medications struggle to penetrate the prostatic tissue effectively, reducing their impact on inflammation and pain. This necessitates longer treatment courses or alternative strategies to enhance drug absorption and promote tissue regeneration. Considering kidney ultrasound can help track the overall health of the urinary system.
The Role of Pelvic Floor Dysfunction
Pelvic floor dysfunction is arguably one of the most significant – yet often overlooked – contributors to chronic prostatitis symptoms. These muscles play a crucial role in supporting pelvic organs, controlling urination and bowel movements, and facilitating sexual function. When these muscles become tight, weak, or uncoordinated, they can compress nerves and blood vessels, contributing to pain, urinary dysfunction, and even erectile difficulties. The connection is often bidirectional: prostatitis causes muscle tension as the body attempts to protect itself, but that very tension then exacerbates inflammation and prolongs symptoms.
- Muscle tightness: Prolonged sitting, poor posture, stress, and previous injuries can all lead to pelvic floor muscle tightening. This creates a pressure gradient within the pelvis, potentially irritating nerves and contributing to prostate discomfort.
- Muscle weakness: Conversely, weakened pelvic floor muscles provide inadequate support, leading to urinary leakage, bowel control issues, and instability in the pelvic region.
- Trigger points: These are hypersensitive spots within the muscle that can refer pain to other areas of the body, mimicking or amplifying prostatitis symptoms.
Addressing pelvic floor dysfunction typically involves a combination of physical therapy techniques, including:
- Manual Therapy: Techniques like myofascial release and trigger point therapy help relieve muscle tension and restore normal movement patterns.
- Biofeedback: This allows patients to visualize and learn how to control their pelvic floor muscles through real-time feedback from sensors.
- Exercise Programs: Tailored exercises strengthen weakened muscles, improve coordination, and promote overall pelvic stability.
Identifying Underlying Contributors
Beyond the prostate itself and pelvic floor dynamics, a deeper investigation into potential contributing factors is vital for successful recovery. These often fall outside traditional medical assessments but can significantly impact symptom severity and persistence.
- Neuropathic Pain: Chronic inflammation can damage nerves in the pelvic region, leading to neuropathic pain – a persistent, burning, or shooting pain that doesn’t respond well to conventional analgesics. Identifying this component requires specialized assessment and may necessitate treatments like nerve blocks or neuromodulation therapies.
- Psychological Factors: Stress, anxiety, depression, and past trauma can all amplify pain perception and contribute to muscle tension. Addressing these psychological components through therapy (cognitive behavioral therapy, mindfulness) is often essential for breaking the cycle of chronic pain.
- Dietary Influence: Certain foods – caffeine, alcohol, spicy foods, acidic fruits – can irritate the bladder and exacerbate prostatitis symptoms in some individuals. Identifying and eliminating trigger foods may provide significant relief. It’s important to consider how urinary pain might change throughout the day.
The Importance of a Holistic Approach
The complex nature of prostatitis demands a holistic approach that moves beyond simply prescribing antibiotics or pain medication. A successful recovery plan should integrate several key components:
- Accurate Diagnosis: Determining the specific type of prostatitis is paramount for tailoring treatment appropriately.
- Multidisciplinary Care: Collaboration between urologists, physical therapists specializing in pelvic health, psychologists/therapists, and potentially pain management specialists can ensure comprehensive care.
- Lifestyle Modifications: Incorporating regular exercise (low-impact activities like walking or swimming), maintaining a healthy diet, managing stress levels, and optimizing sleep are crucial for supporting healing.
- Patient Education: Understanding the condition, its potential causes, and available treatment options empowers patients to actively participate in their recovery journey.
Navigating Setbacks and Maintaining Hope
Recovery from chronic prostatitis is rarely linear. There will likely be periods of improvement followed by flare-ups or setbacks. It’s important to view these as normal fluctuations in the healing process rather than signs of failure. Open communication with your healthcare team, maintaining a positive mindset, and consistently implementing your treatment plan are essential for navigating challenges and staying motivated. Remember that full recovery may not always mean complete symptom elimination, but achieving significant improvements in quality of life is certainly attainable with persistent effort and a tailored approach to care.